How much do you know about dentinal hypersensitivity?
Disclosure: We value transparency at Today’s RDH. This quiz is sponsored content from Dentsply Sirona Preventive as part of our sponsored partner program.
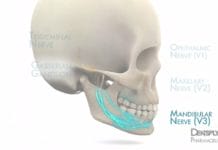
Brännström’s hydrodynamic theory, which describes the mechanism behind dentinal hypersensitivity, states stimulus-induced fluid flow within dentinal tubules activates ________ nerve fibers resulting in the sensation of pain.
The currently accepted theory that describes the mechanism in which pain associated with dentinal hypersensitivity occurs is Brännström’s hydrodynamic theory. This theory describes that stimuli, such as thermal, chemical, tactile, or evaporative, are transmitted to the pulp surface due to the movement of fluid within open dentinal tubules.1 Three types of nerve fibers are found within dentin, including A-delta, A-beta, and C-fibers.2 In this theory, the fluid movement caused by stimuli is thought to stimulate the myelinated, small A-delta fibers, which transmit the sensation of a localized, sharp pain to the brain.1
1. Chung, G., Jung, S.J., Oh, S.B. Cellular and Molecular Mechanisms of Dental Nociception. J Dent Res. 2013 Nov;92(11):948-55. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/23955160.
2. Martens, L.C. A Decision Tree for the Management of Exposed Cervical Dentin (ECD) and Dentin Hypersensitivity (DHS). Clinical Oral Investigations. 2013; 17(Suppl 1): 77-83. Retrieved from https://link.springer.com/article/10.1007/s00784-012-0898-7.
How many tubules can be found in one square millimeter of dentin?
Though it varies from person to person, generally 18,000-21,000 tubules can be found in one square millimeter of dentin. Dentinal tubules are more numerous in the inner third layer than the outer third layer of dentin. The diameter of tubules varies between 2 and 4 micrometers.1
First described by Sir John Tomes in 1850, Tomes’ fibers extend into dentinal tubules from odontoblasts (odontoblastic process) that communicate with tooth pulp. Dentinal fluid within dentinal tubules accounts for about 22% of the total volume of dentin.2 On a weight basis, dentin is less mineralized than enamel (96% in weight) but more mineralized than bone or cementum (about 65% in weight).1
1. Goldberg, M., Kulkarni, A.B., Young, M., Boskey A. Dentin: Structure, Composition and Mineralization: The Role of Dentin ECM in Dentin Formation and Mineralization. Frontiers in Bioscience (Elite Edition). 2011;3:711-735. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3360947/.
2. Davari, A. Ataei, E. Assarzadeh, H. Dentin Hypersensitivity: Etiology, Diagnosis and Treatment: A Literature Review. Journal of Dentistry. 2013;14(3):136-145. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3927677/.
Hypersensitivity is more common among periodontal patients with a reported frequency of 60-98%. The general population reports a lower incidence of hypersensitivity at a rate of 57%.
Hypersensitivity is more common among periodontal patients, with a reported frequency of 60-98%; while a lower incidence of hypersensitivity of 57% is reported by the general population1-3,6. The higher prevalence for this group may be attributed to root surface exposure caused by periodontal disease and treatment.
One study showed before non-surgical periodontal therapy/SRP, between 9% and 23% of patients reported dentinal sensitivity. Over 1-3 weeks following treatment, about 55% of patients reported dentinal sensitivity, and then the sensitivity decreased over time.1
Hypersensitive dentin normally consists of numerous, large dentinal tubules open to the oral cavity with a poorly calcified or absent smear layer. The smear layer is composed of debris from dentrifices, deposits of salivary proteins, and other calcified material that protects cementum and dentin.4 Beyond the removal of the smear layer during non-surgical periodontal therapy/SRP, aggressive instrumentation can remove layers of protective dentin and cementum leading to hypersensitivity.5
1. Chabanski, M.B., Gilliam, D.G., Bulman, I.S., Newman, H.N. Clinical Evaluation of Cervical Dentine Sensitivity in a Population of Patients Referred to a Specialist Periodontology Department: A Pilot Study. J Oral Rehabil. 1997;24:666-72. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/9357747.
2. Von Troil, B., Needleman, E. Sanz, M. A Systematic Review of the Prevalence of Root Sensitivity Following Periodontal Therapy. J Clin Periodontol. 2002;29 (Suppl 3): 173-7. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12787217.
3. Orchardson, R. Gillam, D.G. Managing Dentin Hypersensitivity. J Am Dent Assoc. 2006;137:990-8. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16803826.
4. Martens, L.C. A Decision Tree for the Management of Exposed Cervical Dentin (ECD) and Dentin Hypersensitivity (DHS). Clinical Oral Investigations. 2013; 17(Suppl 1): 77-83. Retrieved from https://link.springer.com/article/10.1007/s00784-012-0898-7.
5. Drisko, C.H. Dentine Hypersensitivity – Dental Hygiene and Periodontal Considerations. Int Dent J. 2002;52:85-93. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/j.1875-595X.2002.tb00938.x.
6. Splieth, C.H., Tachou, A. Epidemiology of Dentin Hypersensitivity. Clin Oral Investig. 2013 Mar; 17(Suppl 1): 3–8. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3585833/.
Parafunctional occlusal forces or occlusal trauma can cause gingival recession which can lead to hypersensitivity. Occlusal trauma never exacerbates the risk of attachment loss in individuals with active periodontal disease.
Parafunctional occlusal forces can be described as when the teeth make contact outside functional activities, such as when chewing food. Parafunctional occlusal forces can cause attachment loss, including gingival recession and bone loss/resorption, due to the excess force placed on the periodontium.
Occlusal trauma, in conjunction with active periodontal disease, can exacerbate the risk of attachment loss (recession). “Excessive functional stress may initiate inflammatory changes in the periodontium and thus enhance destructive bacterial processes.2”
1. Davies, S.J., Gray, R.J.M., Linden, G.J., James, J.A. Occlusal Considerations in Periodontics. Br Dent J. 2001;191:597-607. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11770945.
2. Kemal, U., Zafer, S., Hasan, O. Ismet, D., Sema, H. Severe Gingival Recession Caused by Traumatic Occlusion and Mucogingival Stress: A Case Report. Eur J Dent. 2008: 127-133. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2633168/.
Pathologies that can exhibit similar signs and symptoms of dentinal hypersensitivity include:
Before the diagnosis of dentinal hypersensitivity can be made, differential diagnoses should first be ruled out1. Some of these include:
- Post-restorative sensitivity
- Cracked tooth syndrome
- Fractured restorations
- Marginal leakage/ failing restorations
- Chipped teeth/trauma
- Dental caries/pulpitis
- Post-bleaching sensitivity
- Palatogingival grooves
- Gingival inflammation
- Periodontal pain
1. Martens, L.C. A Decision Tree for the Management of Exposed Cervical Dentin (ECD) and Dentin Hypersensitivity (DHS). Clinical Oral Investigations. 2013; 17(Suppl 1): 77-83. Retrieved from https://link.springer.com/article/10.1007/s00784-012-0898-7.
Gingival recession causing exposed cementum and/or dentin can lead to sensitivity. Causes of gingival recession include:
Gingival recession and the hypersensitivity that can ensue has many possible causes. Some of these causes include1:
- Poor oral hygiene (periodontal disease)
- Improper frenal attachments
- Occlusal trauma
- Anatomy of the labial plate of the alveolar bone
- Aggressive or improper tooth brushing techniques
- Inadequate attached gingiva
- Acute or chronic trauma
- Excessive oral hygiene
- Aggressive instrumentation
- Iatrogenic loss during restorative procedures.
1. Davari, A. Ataei, E. Assarzadeh, H. Dentin Hypersensitivity: Etiology, Diagnosis, and Treatment; A Literature Review. Journal of Dentistry. 2013;14(3):136-145. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3927677/.