Ankyloglossia, also known as tongue-tie, is a congenital anomaly that may severely restrict the tongue’s range of motion. It is caused by an abnormally thick, short lingual frenulum which tethers the bottom of the tongue’s tip to the floor of the mouth. Severe tongue-ties are usually discovered at birth as it interferes with normal breast-feeding.1
If not discovered at birth due to severity, many adults go their whole life unaware of their present condition of tongue-tie, even though they have had a lifetime of dental screenings and checkups. It takes only a few seconds to evaluate for tongue-tie and inform the patient of their condition. During a comprehensive oral exam and oral cancer screening, it is important to lift the tongue for thorough evaluation where we should also check for ankyloglossia.
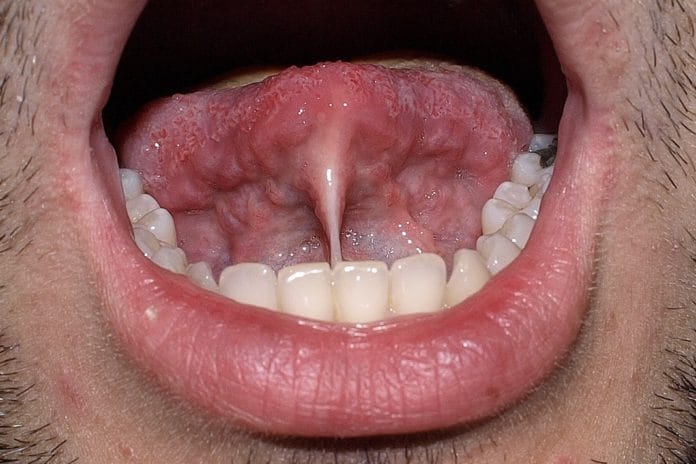
Not all tongue-ties are readily noticed and may require further examination to determine if the patient is limited by their condition. For instance, if you suspect a tongue-tie, but aren’t sure, have the patient open their mouth wide and ask them to reach buccal and distal of their first and/or second molars with the tip of their tongue. If they are unable to access these areas, they should be educated, informed, and presented the option of a lingual frenectomy. The more obvious cases present with a “heart-shaped” pull at the tip of their tongue as the frenulum tugs the midline, and the inability to touch the tip of the tongue to their palate.
Can you imagine growing up being denied the pleasure of licking an ice cream cone? This simple pleasure in itself is worth a frenectomy! Some other notable conditions resulting from ankyloglossia are as follows.
Speech impediment: A myofunctional or speech therapist may take notice of the tongue-tie in young children undergoing speech therapy and give a dental referral for evaluation. A therapist usually notes difficulty in the (l) or (th) sounds as the tongue finds a way to mimic other sounds, but has difficulty producing these sounds due to restriction.
Improper swallowing: Affects oral and whole-body health; digestion, breastfeeding, and possible aspiration.
Improper tongue-rest: Causing a vaulted palate and/or crowding of dentition.
Inability to sweep food particles off teeth: Resulting in a higher rate of decay especially later in life.
Recession: A moderate to severe tongue-tie can cause recession of the gingival margin of the lingual of teeth #24 and #25 as the frenulum chronically pulls on the gingival attachment. This is often mistaken for early-onset periodontal disease.
Social issues: Licking an ice cream cone, “French kissing,” licking your lips, whistling, sticking your tongue out at someone! These are all simple pleasures that may be missed for a lifetime.
Musculoskeletal issues: The tongue being “locked” to the floor of the mouth may also have postural and musculoskeletal implications which could result in poor posture, headaches, TMD, and neck tension.
Conceptualize the idea of being tied down. I recently watched a blog of a young girl who stated that she felt such an immediate burden lifted off her shoulders upon release of her tongue-tie. She stated that she felt alleviated of chronic poor posture, followed by a drastic reduction in tension headaches. A fellow hygiene colleague of mine stated she felt free for the first time in her life after she had a lingual frenectomy. She felt so compelled by her experience, she wrote an action research paper on it.
If the diagnosis and treatment of ankyloglossia is so life-changing, why are we not diagnosing and treating more of them?! Fear. Perhaps we fear the doctor will not back us up. We fear the patient will not be interested. We fear it will be time wasted on our ticking clinical clock. Well, as Franklin D. Roosevelt said, “There is nothing to fear but fear itself.” It seems the only thing really blocking us from noting and suggesting a lingual frenectomy is the fear factor.
I challenge you to inform your doctor/dentist whether or not a patient has tongue-tie, suggest an in-office lingual frenectomy (if the tongue-tie negatively affects the patient’s quality of life), or referral if your doctor prefers to send the patient to an oral surgeon. The worst that can happen is the doctor or patient may not follow-through, but at least you will have peace of mind knowing that you gave your all, and swept fear aside. The best that can happen is you may have a patient who thanks you for changing his/her life!
Observing a lingual frenectomy procedure can appear barbaric, as do so many surgical procedures. The fact is with lasers in the dental office, the frenectomy is done rather easily, and the patient heals rapidly and displays immediate wonder at the movement of his/her tongue! Discussing the benefits of lingual frenectomy procedures with your employer creates an awareness of this undiagnosed condition to the whole dental team.
The next time you lick an ice cream cone, whistle a tune, or stick out your tongue to catch a snowflake, remember what a blessing that freely-movable tongue really is!
SEE ALSO: Geographic Tongue: Is There a Systemic Link?
DON’T MISS: Dental Response to “Sucking a Baby’s Pacifier Clean May Prevent Allergies”