Amalgam tattoos are isolated pigmentations commonly found on the oral mucosa, gingiva, palate, tongue, and buccal and alveolar mucosa. They develop from tiny metal particles found in amalgam restoration material that become embedded in the tissue. In most cases, these tattoos do not cause any health issues or hazards since the mercury from the restorative material is not in a free state.1
Generally, dental patients do not notice an amalgam tattoo in their mouth. It’s usually discovered and mentioned during a dental appointment by a dental clinician.
Amalgam Tattoo Appearance
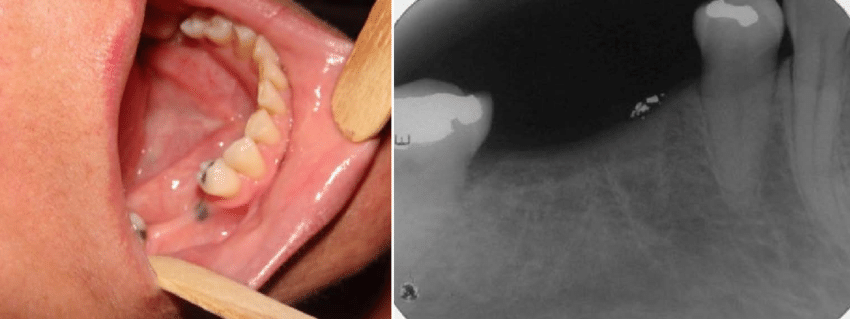
Amalgam tattoos appear as a grey, blue, or black discoloration on the mucous membrane. The lesion will be flat with defined, irregular, or diffuse borders (see Figure 1). Although any mucosal site is possible, the lesions commonly appear on the mandible. The most common sites are on the gingiva and the alveolar and buccal mucosa. Even though amalgam tattoos are harmless, painless, and benign in most cases, they can be mistaken for melanoma.2

Courtesy of Lundin, et al.3
(CC BY 3.0)
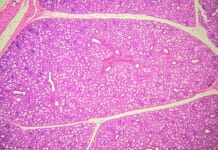
Histopathological features of an amalgam tattoo will show discrete fine, dark granules and irregular solid fragments. These fine, dark granular pigmentations in the lamina propria encase elastic fibers and the basement membrane of the superficial capillaries. Amalgam tattoos “can be found along collagen bundles and vessels and also are found within macrophages, multinucleated giant cells, fibroblasts, and endothelial cells.”1
Amalgam tattoos, like any other foreign body, can cause chronic inflammation. About 38% of people with amalgam tattoos have a foreign body reaction. This reaction is mediated by macrophages (giant cells).4 Giant cell-mediated foreign body reaction occurs at the end stage of the healing process. Chronic inflammation may present as a contact reaction or, in more severe cases, could lead to chronic sinusitis. In most cases, there are no clinical manifestations, and the only evidence of inflammation is determined through histology of the surrounding tissue.5,6
Common Causes of Amalgam Tattoos
Amalgam particles may accidentally and/or traumatically embed into the mucosa, causing an amalgam tattoo during the fitting of crowns, removal of amalgam restorations, extractions of amalgam-restored teeth, endodontic treatment, and flossing shortly after placing an amalgam restoration. “While copper and zinc are rapidly lost from the region of the tattoo, mercury and tin are lost more slowly and, finally, only silver remains permanently in the tissues.”5
Another procedure that may cause an amalgam tattoo is an apicoectomy (also known as root-end surgery). This surgery is needed when an infection continues or develops after root canal treatment, prompting the removal of the apex of the tooth.6 A restoration is placed to seal the root’s apex, and the tissue is placed back over the root to cover it for healing. If amalgam is used as the restorative material, dust particles may tattoo the gingiva.2,7
Amalgam Tattoo Diagnosis
An amalgam tattoo can be diagnosed clinically and sometimes radiographically. As previously mentioned, it’s visually a blue, black, or grey spot on the tissue.3
Radiographically, amalgam tattoos appear radiopaque, the same as an amalgam restoration that appears on a radiograph. However, the metal fragments appear lower on the tooth since it’s located in the tissue (see Figure 2). Amalgam tattoos may not always appear radiographically, but if it does, it confirms the diagnosis of an amalgam tattoo.3
Courtesy of Franca, et al.8
(CC BY 4.0)
If discoloration is localized near a current or a previous tooth that has or had an amalgam restoration, this can help confirm an amalgam tattoo. Once an amalgam tattoo is established, it does not change in size or color and will not blanch with pressure.3
Since the appearance of an amalgam tattoo can resemble cancerous lesions, an amalgam tattoo may easily be mistaken for several different conditions, such as melanoma, pigment-cell nevi, melanotic macules, melanoacanthoma, Kaposi’s sarcoma, and physiologic pigmentation.1
Though oral melanoma is rare, with less than 1% of melanomas presenting on oral tissue, it is a very serious condition. Oral melanomas are most often present on the hard palate (40%) and the gingival surfaces (25%) (see Figure 3). They tend to be diagnosed later in the disease, with 85% being invasive at the time of diagnosis. With a 5-year survival rate of around 15%, it is imperative to consider this as a differential diagnosis when patients present with black, brown, or purple lesions with no radiographic evidence of amalgam remnants. In these cases, biopsy is the best practice as it is the only way to get a clear diagnosis, whether amalgam tattoo or oral melanoma.9

Courtesy of Zahid, et al.10
(CC BY 4.0)
If the darkened area has grown or changed, becomes painful, bleeds, is not located near a tooth, or appears without any recent dental work, a biopsy is warranted to ensure the lesion is not a malignancy.1
If the patient or dental professional notices an unusual spot in the mouth, it’s always recommended to note the lesion by size, color, location, history, pain, and other pertinent characteristics, even if it looks harmless.10
Prevention and Removal of Amalgam Tattoos
Although it’s not a full preventive measure, using a dental dam to isolate treatment areas may decrease the chance of an amalgam tattoo. Having composite fillings placed will prevent an amalgam tattoo.9
In most cases, there is no medical need to remove an amalgam tattoo. However, if it’s a cosmetic concern, the patient may want to have it removed. It can be removed through a laser by gingival ablation.11
Grafting may also be used to cover the amalgam tattoo on the gingiva or mucosa. A combination of grafting and laser treatment can also be done in areas with large amalgam tattoos.12 Another option is surgical removal of the discoloration.1
Conclusion
Though amalgam tattoos are common among patients with a history of amalgam restorations, they should still be documented in their clinical chart. Monitoring these areas to ensure no changes occur is very important since amalgam tattoos resemble many malignant oral lesions.
Advise the patient of the location so they can also monitor it between visits. Any changes should be noted, and the patient should be referred for a biopsy. It is always better to be safe than sorry when it comes to our patients’ health.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Tran, H.T., Anandasabapathy, N., Soldano, A.C. Amalgam Tattoo. Dermatology Online Journal. 2008; 14(5): 19. https://escholarship.org/uc/item/5d43t0x9
- Amalgam Tattoo. (2016). Brigham and Women’s Hospital: Division of Oral Medicine and Dentistry. https://www.brighamandwomens.org/assets/BWH/surgery/oral-medicine-and-dentistry/pdfs/amalgam-tattoo-bwh.pdf
- Lundin, K., Schmidt, G., Bonde, C. Amalgam Tattoo Mimicking Mucosal Melanoma: A Diagnostic Dilemma Revisited. Case Reports in Dentistry. 2013; 2013: 787294. https://doi.org/10.1155/2013/787294
- Muller, S. (2019). Non-Neoplastic Lesions of the Oral Cavity. In L. D. R. Thompson, & J. A. Bishop, Head and Neck Pathology (3rd ed., pp. 175-196.e2). Elsevier Inc.
- Parizi, J.L., Nai, G.A. Amalgam Tattoo: A Cause of Sinusitis? Journal of Applied Oral Science. 2010; 18(1): 100-104. https://doi.org/10.1590/s1678-77572010000100016
- Anderson, J.M., Rodriguez, A., Chang, D.T. Foreign Body Reaction to Biomaterials. Seminars in Immunology. 2008; 20(2): 86-100. https://doi.org/10.1016/j.smim.2007.11.004
- Tatimir, S. (2018, June 12). All about Apicoectomies. Delta Dental. https://www.deltadentalia.com/a-healthy-life/dental-health/dental-procedure-apicoectomy/
- Franca, S., Benevides, R., Martins, C., et al. Oral Manifestations of Chloroquine and Hydroxychloroquine: Differential Diagnoses. Open Journal of Stomatology. 2020; 10(11): 321-332. https://www.researchgate.net/publication/346907967_Oral_Manifestations_of_Chloroquine_and_Hydroxychloroquine_Differential_Diagnoses
- 7 Causes of Black Spots on Gums. (2018, September 18). Healthline. https://www.healthline.com/health/black-gums
- Zahid, E., Bhatti, O., Zahid, M.A., Stubbs, M. Overview of Common Oral Lesions. Malaysian Family Physician. 2022; 17(3): 9-21. https://doi.org/10.51866/rv.37
- Mikami, R., Mizutani, K., Nagai, S., et al. A Novel Minimally-Invasive Approach for Metal Tattoo Removal With Er:YAG Laser. Journal of Esthetic and Restorative Dentistry. 2021; 33(4): 550-559. https://doi.org/10.1111/jerd.12721
- Campbell, C.M., Deas, D.E. Removal of an Amalgam Tattoo Using a Subepithelial Connective Tissue Graft and Laser Deepithelialization. Journal of Periodontology. 2009; 80(5): 860-864. https://doi.org/10.1902/jop.2009.080613