Editor’s Note: The current monkeypox outbreak is an on-going situation. We have made every attempt to ensure this article is up-to-date at the time of publication (July 3, 2022), but some information may have changed since publication. Please visit https://www.cdc.gov/poxvirus/monkeypox/response/2022/index.html for the latest news and information on monkeypox.
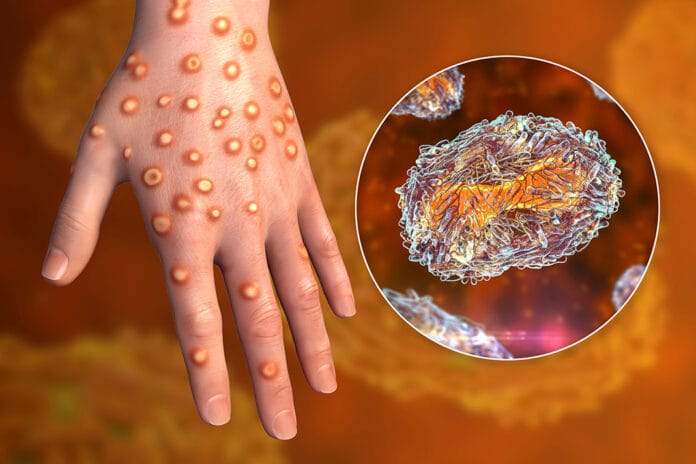
Monkeypox is a member of the Poxviridae family of viruses ‒ an enveloped DNA virus that replicates in the cytoplasm of cells. The most well-known member of the Poxviridae family is smallpox, which was a devastating disease before its eradication on May 8, 1980.1,2 With the recent rise in monkeypox cases worldwide, knowing the signs and how to navigate prevention in the dental setting during the outbreak is crucial to the safety of patients and dental professionals.
The best way to do that is through a better understanding of the disease itself.
Monkeypox Outbreak
Though this may be the first time you have heard about monkeypox in the United States (and in some other countries as well), this is not the first outbreak in this country. In 2003, 47 confirmed cases of monkeypox spread across six states. This outbreak was traced back to pet prairie dogs that were in contact with small mammals from Ghana. This was the first reported outbreak of monkeypox outside of Africa.3
A major difference between the 2003 and current outbreaks is that there were no human-to-human transmissions during the 2003 outbreak. An additional concern regarding transmission is the very real possibility of the virus establishing an animal reservoir (the host in which the pathogen usually persists) outside of Africa, leaving monkeypox as a constant concern in countries that previously had very few to no cases. The spread of the virus within humans and possibly animals allow for mutations that could lead to endemicity.
These are the concerns of health officials and epidemiologists as the outbreak continue.
Monkeypox Transmission
To better understand the significance and length of any infectious disease outbreak, knowing the R-naught (R0) of the infectious disease is imperative. The R0 indicates how infectious a disease is; the goal to end an outbreak is to have the R0 at or below 1.
In the past, monkeypox has been estimated to have an R0 of around 1, indicating that any outbreak should end on its own with minor intervention and mitigation efforts. However, the recent outbreak has perplexed scientists and epidemiologists as it seems to be growing rather than burning out on its own.
Human-to-human transmission was considered rare, but the sheer magnitude of the spread of monkeypox during this outbreak indicates something has changed ‒ not necessarily with the virus but possibly environmental factors. The official R0 of monkeypox is debated but is estimated to be 0.6-1.0 for the Congo Basin clade. However, there is currently no estimate for the West African clade, which is the clade circulating in the U.S., even though it has been estimated to be much lower than the Congo Basin clade R0.
Studies are underway to understand the transmission rate better. It was previously believed that the only possible transmission of the West African clade would be solely due to zoonotic spillover (cross species transmission), with the chance of human-to-human transmission very unlikely.11
Modes of transmission have been identified in the past primarily through animal-to-human contact. Transmission via animals has been identified through scratches, bites, and the consumption of undercooked meat.
All animal reservoirs have not been identified. The natural reservoir of monkeypox has yet to be identified. The disease gets its name because it was first identified in monkeys. However, the natural reservoir is thought to be rodents.4
Human-to-human transmission can occur through close contact with respiratory secretions, skin lesions of an infected person, and contaminated objects, including clothing and bedding. Sexual transmission is suspected, but further studies are needed to confirm this mode of transmission. Transmission via the placenta from mother to child has been documented as well as transmission via close contact with the placenta after birth.4
I want to caution health care professionals from stigmatizing this virus as a sexually transmitted disease that affects one group of individuals. Reports indicate the virus is affecting men who have sex with men at a higher rate than any other group of individuals. However, let us not forget how stigmatizing HIV in this manner led to an epidemic largely due to people refusing to be tested and/or receive treatment. Anyone can be affected by monkeypox. Viruses do not pick a certain demographic to infect at a higher rate. This belief is not only inaccurate but also harmful to efforts to stop the spread of the virus. The only requirement for acquiring monkeypox is to be a vertebrate.
One aspect of good news regarding monkeypox is that it has a relatively low infection fatality rate. The exception to this is, unfortunately, children and immune compromised individuals. The case fatality ratio recently has been estimated between 3% and 6%. However, it can range from 0% to 11%. In comparison, the smallpox case fatality ratio was 30%.4,5
The incubation period ranges from five to 21 days, but the most common incubation time is six to 13 days.
Monkeypox symptoms consist of fever, headaches, chills, muscle aches, exhaustion, swollen lymph nodes, and a rash. The rash begins one to three days after symptom onset. The rash progresses through stages, starting l macules and then progressing through papules, vesicles, pustules, and crusts before falling off. The rash lasts from seven to 14 days. The rash affects the face, palms of the hands, soles of the feet, oral mucosa (70% of cases), genitalia, and conjunctivae.4
The oral lesions have been mistaken for herpes simplex, chicken pox, measles, syphilis, and coxsackievirus (hand, foot, and mouth).6
Demystifying the Monkeypox Outbreak
The cause of the global outbreak is likely due to a shift in the demographics in the sense that many in the population have not been vaccinated for smallpox. The smallpox vaccine provides protection from monkeypox. The smallpox eradication program ended in 1980, with the vaccination of the American public largely ending in 1972, leaving a large portion of the population naive to and unaware of smallpox, making people more susceptible to monkeypox.7
Some conspiracy theories are already circulating regarding the development of a monkeypox vaccine. To clarify, there is no specific vaccine for monkeypox, nor is one being developed. This is because the smallpox vaccine, JYNNEOSÔ, is approved for use in preventing monkeypox in adults 18 years and older. It is administered as a two-dose vaccine with four weeks between vaccine doses. People previously vaccinated for smallpox may only require one dose. Booster doses are recommended at two to 10-year intervals depending on the risk for exposure.8
The United States has a stockpile of this vaccine since public health officials have been concerned that smallpox could be used as a bioweapon. I share this information in the hopes that people will understand the U.S. is not doing anything nefarious. This outbreak is not a political stunt, and securing vaccines to prevent further spread is indeed a responsible public health measure.
The likelihood of the U.S. seeing a mass vaccination program as we saw with COVID is very slim. The vaccines are currently being used for those with a history of exposure and at increased risk of being exposed.
However, this may change in the future as we learn more about the outbreak and if it is determined to be endemic. Additionally, identifying any mutations or animal reservoirs that could easily contribute to another spillover leading to another outbreak may change the protocol.
I think it is important for dental professionals to understand new emerging infectious diseases and the public health response that often shifts as we learn new information. So many dental professionals were caught off guard during the COVID pandemic and the changing public health measures. This was not nefarious; the guidance changed as the experts learned more about the outbreak. You may see much of the same if the monkeypox outbreak is not quickly contained.
As of the writing of this article, there have been 304 confirmed monkeypox cases across 28 states.12 Globally, there are 4,769 confirmed cases in 49 countries.13 On June 23, 2022, a meeting was conducted among the International Health Regulations Emergency Committee members regarding the multi-country monkeypox outbreak. The committee determined the current outbreak of monkeypox does not constitute a public health emergency of international concern (PHEIC).14
However, the national strategy to manage the outbreak includes a vaccine campaign. The U.S. Department of Health and Human Services announced on June 28, 2022, “an enhanced nationwide vaccination strategy to mitigate the spread of monkeypox.”15 This strategy is meant to vaccine those at the highest risk of exposure to monkeypox. Almost 300,000 doses of JYNNEOSÔ will be made available (56,000 immediately and another 240,00 available in the coming weeks). In addition, 750,000 doses will be made available throughout the summer, and 500,000 doses will be made available in the fall.15
The current strategy for vaccination targets “those who had physical contact with someone diagnosed with monkeypox, those who know their sexual partner was diagnosed with monkeypox, and men who have sex with men who have recently had multiple sex partners in a venue where there was known to be monkeypox or in an area where monkeypox is spreading.”15
No strategy has been mentioned regarding the vaccination of health care workers at this time. However, as mentioned, this may change as experts learn more about the transmission of the virus.
Prevention of Monkeypox in the Dental Setting
The WHO has also released infection control and prevention for health care facilities that include the following:10
- Contact and droplet precautions
- Airborne precautions be implemented if aerosol-generating procedures are performed
- Disinfection and sterilization of equipment as per national and facility guidelines
- Linens, towels, and fabric items should be handled and collected carefully
Essentially, continue the preventive measures you have been doing for COVID. COVID is certainly more infectious with a higher transmission rate. Therefore, if you are properly following COVID guidelines for prevention, you should not need to change anything for the monkeypox outbreak at this time.
New emerging infectious diseases will continue to occur as long as we continue to interact with animals. Spillovers happen and are not uncommon. Most of the infectious diseases we see in humans originated in animals.
A spotlight has now been put on infectious diseases due to the COVID pandemic. I think dental professionals should have been paying attention all along to stay aware of outbreaks in their area. Surveillance is ongoing 24/7, 365 days a year, for new emerging infectious diseases.
This is nothing new, and even though you may not have been aware of it, it is what keeps us all safe and prevents pandemics and other outbreaks. This will not be the last outbreak we see in most of our lifetimes. The more you know, the better you will be at disease prevention and control. Infectious diseases are only strong if there is a weak link in the infection cycle. Don’t be the weak link.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
Monkeypox References
- Flint, J., Racaniello, V., Rall, G., Hatziioannou, T., Skalka, A. M. (2020). Principles of Virology (Fifth Edition, Vol. 1). Wiley.
- History of Smallpox. (n.d.). Centers for Disease Control and Prevention. https://www.cdc.gov/smallpox/history/history.html
- U.S. Outbreak 2022: Situation Summary: Past U.S. Cases and Outbreaks. (2022, June 6). Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html
- Monkeypox Fact Sheet. (2022, May 19). World Health Organization. https://www.who.int/en/news-room/fact-sheets/detail/monkeypox
- Ellner, P.D. Smallpox: gone but not forgotten. Infection. 1998; 26(5):2 63-269. https://pubmed.ncbi.nlm.nih.gov/9795781/
- Morbidity and Mortality Weekly Report: Monkeypox Outbreak – Nine States, May 2022. (2022, June 10). Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/71/wr/mm7123e1.htm
- Smallpox: Vaccine Basics. (2017, July 12). Centers for Disease Control and Prevention. https://www.cdc.gov/smallpox/vaccine-basics/index.html
- Smallpox/Monkeypox VIS. (2022, July 1). Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/smallpox-monkeypox.html
- U.S. Outbreak 2022: Situation Summary. (2022, June 29). Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/response/2022/index.html
- Clinical Management and Infection Prevention and Control for Monkeypox. (2022, June 10). World Health Organization. https://www.who.int/publications/i/item/WHO-MPX-Clinical-and-IPC-2022.1
- Alakunle, E., Moens, U., Nchinda, G., Okeke, M.I. Monkeypox Virus in Nigeria: Infection Biology, Epidemiology, and Evolution. Viruses. 2020; 12(11): 1257. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7694534/
- U.S. Outbreak 2022: Situation Summary: 2022 U.S. Map & Case Count. (2022 July 1). Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html
- U.S. Outbreak 2022: Situation Summary: 2022 Monkeypox Outbreak Global Map. (2022, July 1). Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html
- Meeting of the International Health Regulations (2005) Emergency Committee regarding the multi-country monkeypox outbreak. (2022, June 25). World Health Organization. https://www.who.int/news/item/25-06-2022-meeting-of-the-international-health-regulations-(2005)-emergency-committee–regarding-the-multi-country-monkeypox-outbreak
- HHS Announces Enhanced Strategy to Vaccinate and Protect At-risk Individuals from the Current Monkeypox Outbreak. (2022, June 28). U.S. Department of Health and Human Services. https://www.hhs.gov/about/news/2022/06/28/hhs-announces-enhanced-strategy-vaccinate-protect-at-risk-individuals-from-current-monkeypox-outbreak.html