The dental hygienist’s role is often only associated with cleaning teeth and discussing home care habits. Many patients are seen on a rotational basis, and a dental hygienist can easily fall into the habit of running through the same routine, patient after patient. What happens, though, with a patient who describes a set of symptoms with seemingly no clinical evidence?
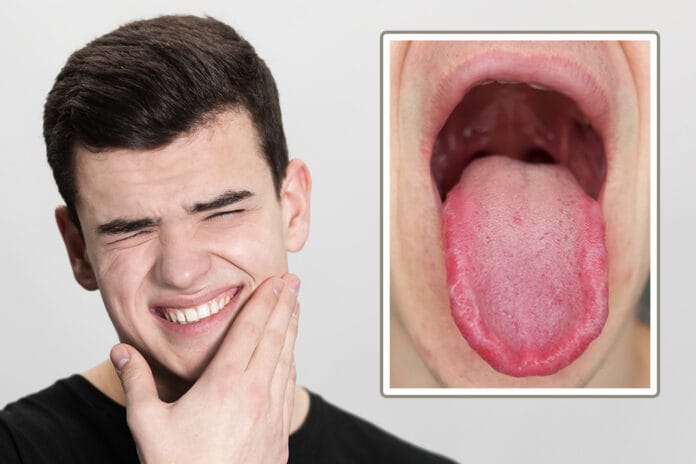
After discussing and updating a patient’s medical history, the discussion shifts to allow the patient to express any concerns. This patient explains that she has recently felt out of sorts and suspects she is nearing menopause. She also explains that her mouth has felt drier for the past several weeks. When she is awake, she feels a tingling and burning sensation in her mouth, but she can’t recall consuming anything hot ‒ let alone anything that would cause these symptoms to last this long.
Your intraoral assessment concludes with no evidence of abnormalities or trauma. After discussing with the dentist, you both concluded that the patient could suffer from burning mouth syndrome.
What is Burning Mouth Syndrome?
Burning mouth syndrome refers to a complex disorder characterized by a chronic or persistent sensation of burning or tingling of the tissues inside the mouth without any easily identifiable cause. For some, symptoms can progress over time, while others report that symptoms began quickly. However, frequency and severity tend to differ from person to person. Symptoms may include sensations of burning, tingling, numbness, xerostomia, and even changes in taste may be noticed. Patients may report feelings similar to being burned from consuming hot foods or drinks, tingling or numbness in the mouth, dry mouth and increased thirst, and altered or loss of taste.1
The presentation of symptoms typically shows in middle age, with females in peri- or post-menopause having three to seven times higher prevalence than men. Overall, occurrence in males is rare before the age of 40.2
What Causes Burning Mouth Syndrome Symptoms?
Although the underlying cause for burning mouth syndrome varies from person to person, the presentation typically involves many of the same neurological functions, which mimic hypertrophy of nerve pathways, resulting in tingling sensations and feelings of xerostomia despite normal salivary function.2
For clearer understanding, Lamey and Lewis categorized the condition based on three generalized factors, ultimately resulting in accompanying disruptions to the body’s response to stressors (hypothalamic-pituitary-adrenal or HPA), changes to the nervous system, psychiatric conditions, and changes in sleep (more specifically disruptions to the circadian rhythm that can distort the perception of pain).2,3
- Type 1: Association with nutritional and endocrine conditions. Symptoms progress and intensify throughout the day.
- Type 2: Association with chronic anxiety. Symptoms remain steady during the day.
- Type 3: Association with food allergies. Unpredictability in symptom occurrence and even no occurrence at times.2
Burning Mouth Syndrome Diagnosis
Diagnosis includes a thorough review of the patient’s medical history, medications, and lifestyle habits.4 Medical history can be telling, for example, because diabetes-associated peripheral neuropathy may cause burning mouth syndrome symptoms.2
A clinical exam should be performed to evaluate intraoral tissues and screen for any evidence of contributing factors, as well as a discussion of patient symptoms, frequency and severity, environmental factors, and assessment of factors that reduce symptoms or make them worse.4
Lab work may need to be ordered, beginning with a complete blood count test that checks several functions such as thyroid, immune function, and glucose. This lab work may help the provider narrow down potential root causes for discomfort in the mouth, such as a recent change in medications or trauma.4
Other tests may need to be conducted, such as allergy testing, salivary sampling, or tissue biopsy for microscopic evaluation of cellular changes that indicate an inflammatory response or allergic reaction. Food allergies that have been associated with burning mouth syndrome include cinnamon, peanuts, chestnuts, and sorbic acid.3 Dental materials that have been associated with being irritants include amalgam, benzoyl peroxide, zinc, methyl methacrylate, and cobalt chloride.2
Additionally, because declines in sleep quality are often linked to burning mouth symptoms, a psychological questionnaire may be administered to identify mental health issues most known to impair sleep.4
Diagnosing burning mouth syndrome is a “diagnosis of exclusion.”2 In other words, the diagnosis comes from narrowing down what the condition is not, ruling out all differential diagnoses. Though this leaves no objective proof that the cause is burning mouth syndrome, no “smoking gun” per se, it is the most plausible diagnosis. “If the cause of the burning symptoms can be justified by any local or systemic conditions, burning mouth syndrome cannot be diagnosed.”2 Further, to diagnose burning mouth syndrome, “the oral mucosa needs to be free of lesions or anomalies.”2
Evaluation criteria for assessment and determining the origin of symptoms:
Five Clinical Criteria2
- Deep and bilateral burning on a daily basis
- Burning pain that lasts at least four to six months
- Severity remains constant or increases throughout the day
- Eating and drinking ease pain
- No sleep interference
Additional Criteria for Consideration2
- Xerostomia
- Sensory changes in the mouth, such as changes in taste or tingling
- Mood or psychological disorders
Primary origin (meaning no original cause found, idiopathic): If no conclusion could be formed about the origin of burning mouth symptoms, the best course of treatment is determined on a case-by-case basis, with the primary goal being pain management, which ranges from pain-relieving medications to salivary substitutes, pain relief oral rinses, or cognitive behavioral therapy.4
Secondary origin (caused by environmental, lifestyle, or internal factors): Treatment is much more specific when the secondary cause(s) is known. For example, oral infections and allergies to medications, foods, or dental products can be resolved with appropriate treatments such as antibiotics or adjustments in diet and/or medications.4
Burning Mouth Syndrome Treatment
Treatment for burning mouth syndrome and management of symptoms can be complex, partly because there are many possibilities for differential diagnoses, ranging from stomatitis, neoplastic lesions, herpes simplex or herpes zoster, or pemphigus.2
After a thorough evaluation of such things as poor sleep, food or drink triggers, or infection (i.e., candidiasis, H. pylori), patient education is greatly important to ensure avoidance of symptomatic triggers. Some of the triggers can be managed to achieve a complete resolution of symptoms. Emphasizing compliance with treatment recommendations will provide the patient with greater confidence and control in maintaining a greater quality of life.
Typical medications prescribed range between topical and systemic, depending on the suspected cause for symptoms.
Topical Medications for Burning Mouth Syndrome2
- Capsaicin is derived from chili pepper and used as a topical analgesic. However, it may not be successful for some due to the tendency for toxicity, causing difficulty in swallowing and a temporary increase in burning upon application. Systemic prescription has been known to cause gastric discomfort and is advised to be used with caution.
- Topical clonazepam is administered as a dissolvable lozenge and taken three times daily for two weeks. Symptoms have been reported to recur after completing the two-week regimen, as well as xerostomia and fatigue.
- A mouth rinse of hot sauce and water has been reported to improve symptoms, as well as a topical application of 70% aloe vera gel three times daily.
- Topical lidocaine is not recommended for symptom relief due to its short-term effectiveness.
Systemic Medications for Burning Mouth Syndrome2
- Clonazepam is an anticonvulsant that can be prescribed as a short-term aid to relieve burning mouth pain but does not have any effect on taste or salivary dysfunction.
- Antidepressants, SSRIs, and antipsychotics can be used as another short-term treatment for the burning symptoms.
- When used by peri- or post-menopausal women, hormone replacement therapy has shown a decrease in symptoms.
- One of the greatest reports for symptom management is shown with the supplementation of vitamins B, C, B12, folic acid, and minerals. Not only were symptoms completely resolved, but levels of components in the blood called serum homocysteine and hemoglobin, known for their roles in vascular health and function, also improved. It’s important to note, however, that additional testing would be necessary to rule out evidence of elevated homocysteine levels, as further increasing this can exacerbate pre-existing hypertension symptoms and greatly damage bodily organs.5
Management of symptoms is key to maximizing the patient’s quality of life and prevention of caries. Burning mouth creates increased susceptibility to caries when the salivary function is impaired, causing changes to the diet in an attempt to ease symptoms.6
In Closing
With the understanding that burning mouth syndrome is difficult to care for, dental hygienists are key in encouraging clear communication and honest feedback to best manage discomfort and prevent unwanted outcomes.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Burning Mouth Syndrome. (2022, September). NIH: National Institute of Dental and Craniofacial Research. https://www.nidcr.nih.gov/health-info/burning-mouth
- Bookout, G.P., Ladd, M., Short, R.E. (2023, January 29). Burning Mouth Syndrome. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK519529/
- Smith, S.M. The Role of the Hypothalamic-pituitary-adrenal Axis in Neuroendocrine Responses to Stress. Dialogues Clin Neurosci. 2006: 8(4); 383-395. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181830/
- Burning Mouth Syndrome. (2023, February 22). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/burning-mouth-syndrome/diagnosis-treatment/drc-20350917
- Ganguly, P., Alam, S.F. Role of Homocysteine in the Development of Cardiovascular Disease. Nutr J. 2015; 14: 6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4326479/
- Castillo-Felipe, C., Tvarijonaviciute, A., Lopez-Arojna, M., et al. Response to Treatment with Melatonin and Clonazepam versus Placebo in Patients with Burning Mouth Syndrome. J Clin Med. 2022; 11(9): 2516. https://www.mdpi.com/2077-0383/11/9/2516