
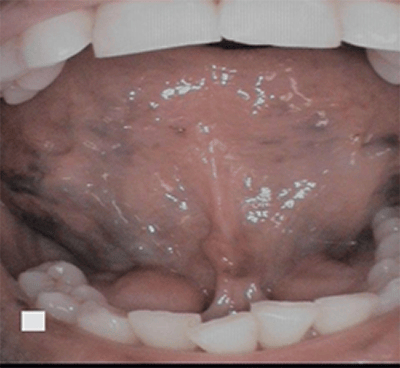
Caviar tongue is a condition recognized by purplish veins located on the ventral side of the tongue. Veins are normally visible underneath (ventrally) the tongue since the mucous membrane is so thin and translucent. However, with caviar tongue, the blood vessels become dilated and tortuous and appear round and black (resembling caviar).1
Caviar tongue is also referred to as sublingual varices (plural) and varix (singular) and look like varicose veins in the tongue (see Figure 1). It is a benign, asymptomatic, venous lesion.1
Caviar Tongue Location
Caviar tongue occurs in a few different sites. It is commonly noticed under the tongue along the sublingual vein, the floor of the mouth at the opening of the sublingual glands, and along the lateral, ventral (underside) of the tongue. It’s rarely seen on the lips and buccal mucosa.
It originates as small outpouching of the veins and gradually elevates the overlying thin mucosa varying from red to purple, resembling buckshot (see Figure 2) or caviar with an iridescent surface.1 They originate bilaterally from the posterior of the tongue and end at the apex of the tongue.2 Histologically, a sublingual varix is a dilated vein with no inflammatory changes. The endothelium is hypoplastic, and the wall is thick and cellular.

Due to the dilated blood vessels, the flow of blood will slow down, causing a higher risk for thrombosis. A regular varix will blanch on compression. A varix with a thrombosis will not blanch under compression due to the thrombus unable to be pressed into the adjacent vasculature. A varix will feel firmer, similar to a BB pellet, beneath the mucosal surface.
Although this sounds serious, it poses very minimal risks of embolism.3
Risk Groups for Caviar Tongue
Caviar tongue is seen most commonly in 40 years of age and older, affecting 10% of the population with increased frequency into life, with the highest occurrence during the eighth decade.1,4 The aging process leads to a weakening of the venous wall from degeneration of elastic fibers.
The lesions are commonly seen as a physiological change in connection with age.4 During the aging process, the changes with the blood vessels and connective tissue in blood flow may change the arterial pressure at the arteriovenous shunts. The process of the smooth muscle fibers encircles the capillaries and arterioles at periodic locations, causing the opening and closure of vessels. This activity changes the distribution of blood in the tissues causing blood to pool from arterioles to the venules without passing the capillary bed.4,5
Although bleeding is uncommon, bleeding from a tortuous vein may be found in association with conditions such as increased venous pressure (portal hypertension) or superior vena cava syndrome.1 Portal hypertension is high blood pressure in the hepatic portal system. The portal vein is the vein that carries blood from the digestive organs to the liver. This increased pressure in the portal veins may lead to swollen veins throughout the body. A possible connection of portal hypertension and varicose veins of the leg to sublingual varices has been suggested.5
Superior vena cava syndrome is multiple symptoms that result when blood flow through the superior vena cava − the large blood vessel that returns blood from the upper body back to the heart − is blocked. When this occurs, swelling of the face, neck, and dilation of the veins on the skin surface occurs.6
Caviar Tongue Etiology
As to what else causes the larger, prominent blood vessels underside the tongue is not fully concrete. Other conditions have been studied and researched with a variety of studies including sublingual varices associated with smoking, diabetes mellitus, hypertension, chronic cough, venous insufficiency, vitamin C deficiency, denture wearing, and cardiovascular and cardiopulmonary disease. All have been suggested as predisposing factors, but researchers are unable to solidly prove it.2
A Saudi Medical Journal study focused on correlations or predisposing factors of sublingual varices with smoking, cardiovascular conditions, hypertension, denture wearing, and vitamin C deficiency.3 According to this study, a patient 40 years of age and older with sublingual varices has a 50% risk of being hypertensive. If smoking is involved, the risk increases to 58%. In this group of people studied, the prevalence of sublingual varices associated with age, smoking, and hypertension were higher (64.7% of smokers compared to 44.7% of nonsmokers).3,4
Older studies show strong associations with cardiovascular disease, but some studies found no relation.3 Sublingual varices were found connected to vitamin C deficiency while the denture wearing and diabetes connection to sublingual varices have not been sufficiently proven.4
If caviar tongue is present in younger people, it is suggested that it could be a sign for premature aging. It may be an underlying systemic disease. Another study found that healthy, non-medicated people ranging between 20 to 95 years of age had no oral changes with the tongue. Although age-related sublingual varices may be associated with systemic diseases, malnutrition, medication, and ill-fitting dentures.3,4
While writing this, I did my own “clinical study” with patients. I found 100% of my patients who had caviar tongue were also on high blood pressure medication. It could be a coincidence. It could be substantial or faulty. Either way, it’s something to be aware of. While the study from above confirmed the prevalence of sublingual varices with hypertension Mentioning this condition to a patient may be beneficial for the patient to be aware of their blood pressure and systemic health.
Now Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Viswanath, V., Nair, S., Chavan, N., Torsekar, R. Caviar tongue. Indian J Dermatol Venereol Leprol. 2011; 77: 78-9. Retrieved from http://www.ijdvl.com/text.asp?2011/77/1/78/75002.
- Akkaya, N., Olmez, D., Ozkan, G. Evaluation of the factors associated with sublingual varices: a descriptive clinical study. Folia Morphological. Retrieved From https://pdfs.semanticscholar.org/c293/3d66c8974d1ea60ee99ddf926e205fab498e.pdf.
- Neville, B.W., Chi, A.C. Developmental Defects of the Oral and Maxillofacial Region. Color Atlas of Oral and Maxillofacial Diseases. Retrieved from https://www.sciencedirect.com/topics/medicine-and-dentistry/varices
- Al-Shayyab, M.H., B.aqain, Z.H. Sublingual varices in relation to smoking, cardiovascular diseases, denture wearing, and consuming vitamin-rich foods.” Saudi medical journal. 2015; 36(3): 310-5. doi:10.15537/smj.2015.3.10429.
- Hedström, L., Albrektsson, M., Bergh, H. Is there a connection between sublingual varices and hypertension? BMC Oral Health. 2015; 15(78). Retrieved from https://doi.org/10.1186/s12903-015-0054-2.
- Wedro, B. Superior Vena Cava Syndrome. Retrieved from https://www.medicinenet.com/superior_vena_cava_syndrome/article.htm#what_is_superior_vena_cava_syndrome.









