It is, of course, common knowledge to all of us in the dental profession that systemic diseases can be exacerbated or even caused by negligent dental hygiene and related oral health diseases. But, did you know that, as a dental professional, you may notice various side effects of certain diseases that the patient doesn’t realize that they have?
Ankylosing Spondylitis
Dr. Craig Gimbel, DDS, is a retired dentist and member of the board of directors of the Ankylosing Spondylitis Association, who now researches the effects that the disease has on a sufferer’s dental condition, which he explores in his general article, Ankylosing Spondylitis and Dentistry. Ankylosing spondylitis, or AS, is a dangerously under-diagnosed autoimmune disease that many doctors mistake for either general arthritis or osteoarthritis when, unfortunately, it is so much more.
Have you heard of ankylosing spondylitis? Perhaps you have not as most people haven’t.
To diagnose this disease, the patient themselves must recognize the symptoms and specifically ask for a specialized blood test that many doctors aren’t even aware exists. Due to the nature of the disease, dental professionals may easily observe many symptoms of the disease and can suggest a visit to a doctor or rheumatologist to request the test.
Noticeable Symptoms
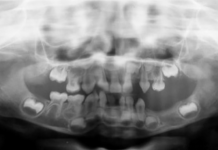
AS causes inflammation throughout the body, including the TMJ, directly causing TMD, especially the clicking of the jaw when opened and the loss of bone, and thus, teeth. AS restricts the movement of the rib cage and therefore causes respiratory problems that become evident in the dental chair specifically due to the supine position during treatment.
A person suffering from AS will also have problems laying back in the chair due to spinal stiffness, extreme pain, and calcification of the spine that can eventually cause a debilitating hunched back that makes dental hygiene maintenance difficult, even impossible.
A person with AS has limited neck movement and may not respond well to any form of anesthesia due to decreased lung function and various heart problems that the sufferer may not be aware that they have developed due to this disease. This may lead to terrifying and life-threatening medical emergencies during dental treatment.
The Dental Chair
AS forces a sufferer to move almost constantly, even when asked to sit still during dental treatment because they must constantly readjust the position of their shoulders, neck, and spine. Due to the usual diagnosis of TMD, opening the mouth wide enough for hygiene or restorative treatment may be difficult or even impossible and recovery time after a procedure lasts much longer due to the normal inflammation always present.
Dental procedures that expose bone may not heal, causing the death and deterioration of the bone, called osteonecrosis. Orthodontic interventions in adults, when the disease first presents itself, can take much longer and cause double the pain that an average adult would experience during treatment. Bone calcification causes the teeth to move slower as the teeth may have to ‘breakthrough’ various deposits of growth.
There is no medication to fix AS and the sufferers must take biologics created for other diseases, such as cancer, that further suppress their immune systems. Even the best infection control protocols within a dental practice may still spread life-threatening bacteria to these patients, the same as organ transplant patients and those taking immune-suppressant medication. Scheduling immune-compromised patients with the first appointment of the day, when aerosols are at their lowest in the dental office, maybe the safest.
Secondary Sjogren’s Syndrome
AS can cause secondary Sjogren’s syndrome, which is an autoimmune, connective tissue disorder that affects the salivatory glands that will, as we know, negatively affect their dental health. The sufferer will have an extremely dry mouth that disrupts healing, causes ulcers, and fungal infections (candidiasis), while the enamel on their teeth begins to decalcify.
Decay is especially noticeable along the gingival margin and dental professionals are usually the first to notice the symptoms. Dental professionals may be able to suggest, or even prescribe, medications that will alleviate xerostomia and aid in healthy oral hygiene. Patients with AS have a very high risk of periodontal disease.
Most immune-related, systemic problems are more evident in the mouth, where symptoms may appear first, than in a person’s general appearance. AS is yet another condition that shows it is abundantly helpful if patients are open and honest with their medical history when in the dental office. If you suspect that they may be suffering from a disease, like AS, while you cannot diagnose them, you can list the symptoms you see and refer them to their primary care physician for the proper testing. Communication not only bridges the gap between dental and medical professionals but may also save the bodies and lives of your patients.