Heartburn, acid reflux, and GERD are often used reciprocally as they are stages of each other. The initial signs of any digestive issue may be heartburn. As conditions progress in the digestive process, acid reflux will start to appear more frequently. If that doesn’t resolve or settle down, a chronic condition known as GERD becomes a lifetime event.
Dentally, it’s important to know these conditions since they can cause permanent damage to the teeth. Erosion of the teeth is a classic sign that dental professionals will notice in the oral cavity.
Heartburn
Heartburn can cause pain in the chest. It occurs within the digestive system and happens after meals, specifically in the esophagus. The lining of the esophagus is more fragile than the lining of the stomach. When the acid stays in the esophagus, it causes a burning sensation in the chest. The pain is a sharp, burning, or tightening sensation, concerning enough to mimic heart pain because it’s often mistaken for heart attack pain. Heartburn may resemble an uncomfortable or burning sensation that moves up around the neck and throat, making it feel like it’s located behind the breastbone.1
Heartburn is prevalent, existing in about 60 million people a month.1 It mainly occurs after eating, especially after a big meal. Bending over or lying down tends to worsen it. This can be managed by avoiding fatty, spicy, or acidic foods, losing weight, and quitting smoking. Mild, infrequent heartburn is usually treated with antacids.
Antacid’s functions are to help neutralize stomach acid. Common brands are Alka-Seltzer, Maalox, Mylanta, Rolaids, and Tums. Antacids are not meant for long-term use or on a regular basis as they can have a laxative effect, develop sensitivities to certain foods or develop an allergic reaction. They contain calcium, so using them quite often may cause too much calcium intake, which may lead to nausea, vomiting, kidney stones, mental changes, and alkalosis.
If it seems like these medications are being used more often, then it may no longer simply be heartburn and could be acid reflux or GERD.2
Important to note if taking antacids:
-By neutralizing stomach acid, any antacid can interfere with the absorption of iron, zinc, and possibly other minerals.8
-Aluminum-containing antacids can bind with phosphorus and interfere with its absorption, and this can lead to further calcium depletion.8
-Calcium-containing antacids may also compete for absorption with iron. Even though calcium antacids may alter the absorption of magnesium, the clinical importance of this effect appears to be minimal.8
-When taken with zinc supplements, calcium-containing antacids might substantially decrease zinc absorption. However, eating a meal appears to mitigate this effect.8
-Calcium antacids might also impede the absorption of manganese and chromium.8
-Citrate may increase aluminum absorption: Concerns have been raised that the aluminum in some antacids may not be healthy. Since there is some evidence that calcium citrate supplements might increase the absorption of aluminum, it may not be a good idea to take calcium citrate at the same time of day as aluminum-containing antacids. To avoid this, taking other forms of calcium or avoid antacids containing aluminum.8
Acid Reflux
Acid reflux is when the acid from the stomach moves backward into the esophagus, irritating the tissue. The lower esophageal sphincter muscle connects the esophagus and the stomach. This muscle tightens the esophagus after food passes into the stomach. If the lower esophageal sphincter muscle doesn’t tighten or becomes weakened, the acid from the stomach flows into the esophagus.
Symptoms of acid reflux are heartburn, cough, sore throat, a burning and pressure sensation in the breastbone area, bloating, sour taste in the mouth and a bitter taste in the back of the throat, difficulty swallowing, tightness in the throat, and the feeling of food stuck in the throat.1
Management is related to food changes and habits. Avoid eating close to bedtime, don’t lie down after eating, avoid large meals, and stick to smaller, more frequent meals. Also, avoid fatty, greasy, caffeine, chocolate, mint, spicy, citrus, and tomato-based foods.
Medications suggested are antacids or histamine-2 receptor blockers. The latter is stronger than antacids, and they reduce the amount of acid the stomach produces by blocking histamine, which tells the stomach to produce acid. These medications are Tagamet, Pepcid, Zantac, or Axid.3 Histamine-2 receptor blockers are meant for short-term relief of up to two weeks of acid reflux and may relieve mild GERD symptoms.
If these medications are unproductive, then proton pump inhibitors will be diagnosed to reduce acid production by blocking the enzyme in the stomach wall that produces this acid. These medications are Nexium, Prevacid, Aciphex, and Protonix.4
Promotility agents may be used by stimulating the gastrointestinal tract muscles to help prevent acids from staying in the stomach for too long. Included in the function is strengthening the lower esophageal sphincter to help stop reflux into the esophagus. These medications encompass metoclopramide and bethanechol.
Coating agents such as sucralfate may be prescribed to treat ulcers that may develop with acid reflux.1
GERD
GERD, gastroesophageal reflux disease, is the chronic form of acid reflux. GERD is considered when acid reflux occurs more than twice a week or causes inflammation in the esophagus. While heartburn and acid reflux is considered a periodic acute condition, GERD is chronic. At this stage, doctors need to promote the management of long-lasting habits ad examine a person’s anatomy that may generate GERD.1
Symptoms of GERD are bad breath, tooth enamel damage, regurgitation, chest pain, heartburn, persistent dry cough, and trouble swallowing. Sources to increase GERD’s risk are extra weight, which puts pressure on the stomach, hiatal hernia, which reduces the pressure of the lower esophageal sphincter, smoking, alcohol consumption, and even pregnancy. Certain medications include antihistamines, calcium channel blockers, pain relievers, sedatives, and antidepressants may weaken the lower esophageal sphincter causing stomach acid to travel through.1
Relief of GERD in relation to acid reflux management are weight loss, smoking, and alcohol cessation. Although there doesn’t seem to be a special diet for GERD, dietary modifications such as avoiding high-fat foods, caffeine, chocolate, onions, peppermint, carbonated drinks, alcohol, citrus, or tomato-based products may be beneficial.
GERD is a long-term chronic condition that varies in severity. The severity correlates with the degree of damage to the lower esophageal sphincter. Once the lower esophageal sphincter is damaged, it’s permanent and cannot be reversed. The severity of reflux is determined by the frequency, volume, and duration of reflux occurrences.5
Stages of GERD
Stage 1 Mild GERD: Minor damage to the lower esophageal sphincter with occasional acid reflux episodes. Symptoms are controlled easily by over-the-counter heartburn medications. Quality of life is unaffected.5
Stage 2 Moderate GERD: More extensive damage to the lower esophageal sphincter with frequent and higher intensity episodes. Symptoms are now chronic, and long-term acid-suppressive medications are needed to manage the symptoms. Interferes more regularly with quality of life.5
Stage 3 Severe GERD: Erosive GERD is present, and a significant risk of Barrett’s esophagus is more attainable. Prescription level acid-suppressive medications aren’t able to suppress the symptoms anymore as regurgitation is more frequent. Surgery is a high probability at this point, as the quality of life has lessened substantially. Drug treatment has very minimal if any effect as surgical repair of the lower esophageal sphincter is this most beneficial option to improve symptoms and quality of life.5
Stage 4 Pre-cancerous condition or reflux-induced esophageal cancer: This stage is the result of several years of acid reflux, affecting 10-15% of long term suffers progress to this advanced case. The lining of the esophagus is damaged to the point of cellular changes for the development of pre-cancer. This condition is Barrett’s esophagus, which increases the risk of developing acid-reflux induced esophageal cancer. At this degree, narrowing of the esophagus may happen causing a sensation that food is sticking in the esophagus, along with burning in the throat, chronic cough, and hoarseness.5
Barrett’s Esophagus
Barret’s esophagus is attributed to long-standing GERD. It is accompanied by heartburn or regurgitation and may generate changes in the cell lining of the esophagus. As Barrett’s esophagus is associated with a risk of developing esophageal cancer, it’s important to have thorough checkups with a medical doctor. Imaging and biopsies are needed to diagnose Barrett’s esophagus and to check for pre-cancerous cells. Treatment recommended is to help prevent esophageal cancer.5
Those who have Barrett’s esophagus usually do not have reflux symptoms, also described as “silent reflux.” Other symptoms may be difficulty swallowing food, frequent heartburn, regurgitation, and chest pain. If it’s been several years with symptoms having a medical exam for Barrett’s esophagus is highly recommended. Risk factors are family history, current or past smoking, chronic heartburn, and acid reflux that do not improve with medications. In addition, being overweight, white, male, and over 50 years of age are contributors.5
GERD in Children
GERD can happen within any age group. With infants, it’s quite common for contents to reverse back into the mouth; they have smaller stomachs and unable to tolerate fullness as well. Within the first two months of life, up to 80% of infants will have regurgitation, and then it tends to taper off. Within the first year, 95% of infants will outgrow it.1
Symptoms in children include bad breath, chest and abdominal discomfort, frequent respiratory infections, heartburn, and a hoarse voice. If a child has those symptoms regularly, it’s important to recommend they see a pediatrician as experiencing this when they’re young can increase the risk of permanent esophagus damage.1
GERD During Pregnancy
While pregnant women commonly experience heartburn and GERD, the good news is that it goes away after the baby’s birth. A pregnant woman initially experiences GERD in the first trimester, which may worsen by the third trimester. During pregnancy, progesterone’s increased levels may cause the lower esophageal sphincter to relax, allowing acid reflux more flexibility. Furthermore, increased pressure on the stomach from the growing uterus could expand the likelihood of GERD.
During pregnancy, management is avoiding the same foods as stated previously and sleeping with the head slightly higher as medications are to be avoided as they may pass onto the fetus.1
Inflammatory Reaction
A study in the Journal of the American Medical Association by Kerry Dunbar, MD, PhD, suggests stomach acid isn’t what’s damaging the esophagus, but it’s the inflammatory response that’s causing the damage. The study results revealed the esophagus didn’t show chemical burns from acidity, but rather white blood cells, inflammatory proteins, and cytokines to suggest more of an injury the body is trying to self-heal.6
Oral Health
Patients who announce they have some form of acid reflux may not be aware of the damage it slowly does to the teeth. Acid reflux is one of the main causes of tooth erosion and can lead to thin, sharp, and pitted teeth.7 When acid bathes the teeth and sits there for minutes at a time and frequently throughout the day, it ultimately destructs the tooth anatomy.
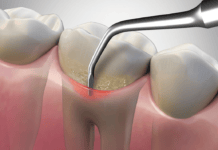
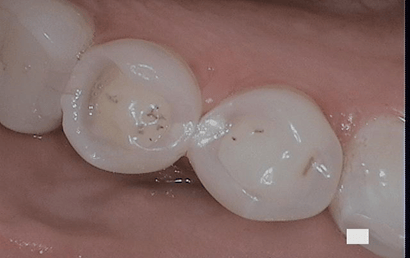
With tooth erosion being permanent, recognizable conditions that come from it are a yellowish discoloration of the teeth, cupping, crater (see Figure 1), or flattening appearance, fillings that have worn, an increased risk of cavities, and pain or sensitivity with a thinner enamel or exposure of the dentin.
Keep in mind erosion of the teeth may not be from acid reflux. It could be from other conditions such as diet, eating disorders, environmental factors, and certain medications.
Managing oral health with patients with acid reflux is a constant battle. Advising a patient to wait to brush at least 30 minutes after an episode will lessen the assault on the tooth structure. Because the saliva can only buffer and neutralize the acid so much, encouraging the patient to rinse with water, mouth wash, and using xylitol and fluoride products is also beneficial.
The appropriate restoration to fix tooth erosion depends on the structural damage of the tooth. If the tooth has eroded sufficiently, simple restorations alone may not be the solution. If the erosion is deep into the tooth, affecting the dentin, then a crown or even a root canal may be necessary. Some teeth may be beyond saving; in that case, an extraction would be the best procedure.
With the progression of having acid reflux, the symptoms and treatments seem to interrelate, whereas the quality of daily life may become more cumbersome. Having a thorough health history will determine if acid reflux is a concern and if tooth erosion is created from that or other conditions. Tooth erosion doesn’t happen overnight; it’s a repeated exposure over a duration of time. Once the damage is done, it’s permanent and irreversible; therefore, the goal is maintaining the health of the tooth structure. Educating the patient on preventing more deterioration and treating sensitivity will change the patient’s quality of life immensely if that’s a concern.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Kinman, T. (2020, April 9) What Are the Differences Between Heartburn, Acid Reflux and GERD? Retrieved from https://www.healthline.com/health/gerd/heartburn-vs-acid-reflux
- Haskins, J. (2019, July 2). Antacids. Retrieved from https://www.healthline.com/health/antacids#interactions
- Histamine 2 Blockers Curb Acid Production. (2016, February 29). Explore Health. Retrieved from https://www.health.com/condition/gerd/proton-pump-inhibitors-fight-acid-reflux
- Munha, J.P. (n.d.). Heartburn vs. Acid Reflux: How to Tell the Difference. Medicine Net. Retrieved from https://www.medicinenet.com/heartburn_vs_acid_reflux_differences_similarities/article.htm#how_are_heartburn_and_acid_reflux_treated
- Cox, L. (2018, November 15). The Progressive Stages of GERD. Reflux MD. Retrieved from https://www.refluxmd.com/the-progressive-stages-of-gerd/
- Hamilton, C. (2016, May 18). Have GERD? Stomach Acid May Not Be the Only Cause, Study Says. Explore Health. Retrieved from https://www.health.com/condition/gerd/inflammation-not-acid-reflux
- Dotinga, R. (2012, March 8). Acid Reflux from Chronic Heartburn May Damage Teeth. Medicine Net. Retrieved from https://www.medicinenet.com/script/main/art.asp?articlekey=155719
- (n.d.). Beth Israel Lahey Health Winchester Hospital. Retrieved from https://www.winchesterhospital.org/health-library/article?id=21407