
The purposes of a thorough patient health history are discussed by Vavrosky.1 When that thorough health history is combined with an educational session tailored to patients’ needs, they will receive the kind of help that a dental hygienist is well trained to share. Snyder discusses how periodontitis can link to diabetes and vice versa.2
This paper builds upon the works of Vavrosky and Snyder to emphasize the importance of a thorough health history along with patient education to help patients who have either periodontal disease or diabetes (or both) understand the potential seriousness of these diseases since both are now worldwide epidemics.
The three major ongoing epidemics in the world fall directly into the realm of dental hygienists ‒ periodontal disease, diabetes, and obesity. It is important to learn why obesity is a third worldwide epidemic that links to the other two. Dental hygienists’ education makes them their patient’s ideal first line of defense for understanding advice on all three epidemics.
Why Are They Epidemics?
Since the early 1990s, diabetes and periodontal disease have been labeled as worldwide epidemics due to the exponential increase in infected people. In 2020, an estimated 463 million people worldwide already live with diabetes. That’s 6% of the world’s population, or one out of every 17 of the earth’s human inhabitants ‒ a number predicted to increase to over 700 million by 2045.3 It is already one of the world’s top 10 causes of death. In the U.S., one out of 10 Americans, or 34.2 million people, have diabetes, but an unbelievable one out of five Americans don’t even know they have it!4
The incidence of periodontal disease has continually increased during the past three decades, making it the 12th most frequent pathology worldwide. Current epidemiological estimates of periodontal disease support the portrait of a growing epidemic.5 In the U.S., half of American adults aged 30 and older have periodontal disease. In U.S. adults ages 65 and older, the rate increases to 70%.6
It’s a Three-way Street
Ongoing research has linked the interaction between obesity, periodontal disease, and diabetes, making the journey a three-way street (see Figure 1).7 Not only are people with diabetes more susceptible to periodontal disease, but it has the potential to affect the control of blood glucose, which would contribute to diabetic progression. When you add obesity into the mix, it gets worse. A worldwide epidemic of obesity has tripled since 1975. The definition of obesity is based on the body mass index (BMI), which is a person’s weight in kilograms divided by the square of that person’s height in meters.
In 2016, over 650 million people worldwide were categorized as obese; almost 9% or one out of every 11 of the earth’s human inhabitants were obese.8
To calculate your BMI, divide your weight in pounds by the square of your height in inches; then multiply that result by 703.1 to convert to kg/m2. For example, a 150-pound person who is 5 feet 7 inches tall has a BMI = (150/ 672) times 703.1 = 23.5. For convenience, see Table 1 for both metric and English equivalents to BMI values.
| BMI (kg/m2) | BMI (pounds/inch2) | Body Weight Status |
| Below 18.5 | Below 0.026 | Underweight |
| 18.5 – 24.9 | 0.026 – 0.035 | Healthy |
| 25 – 29.9 | 0.036 – 0.043 | Overweight |
| 30 and Above | 0.044 and Above | Obese |
Table 1. BMU for Adults Age 20 and Over 9
Explaining the Interactions to Patients
The remainder of this article contains highlights of explanations I’ve used with my patients over 25 years to help them understand periodontal disease, diabetes, and obesity. I’d adjust the degree to which I use a technical explanation depending upon whether my patient is someone like an engineer with a keen interest in detail or someone who just needs it explained in simple terms to help them understand the basics.
The ability of a hygienist to sense what level of detail to use with a patient will make a huge difference in connecting with them and “seeing the light go on.” Remember, if you lose the patient with a poor explanation, you’ve really both lost. Our hygiene team used these and similar techniques over many years. We were quite successful in both uncovering diabetes that the patient was unaware of (based upon their symptoms) and in successfully treating and/or controlling a patient’s periodontal disease.
How obesity affects diabetes and gingiva ‒ Fat cells (adipocytes) are inflammatory. They produce and secrete proinflammatory cytokines such as tumor necrosis factor alpha (TNFα) and interleukin 6 (IL-6).10 The increased levels of these cytokines can cause insulin resistance, high blood sugar, and breakdown of the bone supporting teeth.7 (Cytokines are small proteins whose function is regulation of inflammation. Some cytokines stimulate and some slow down the immune system.)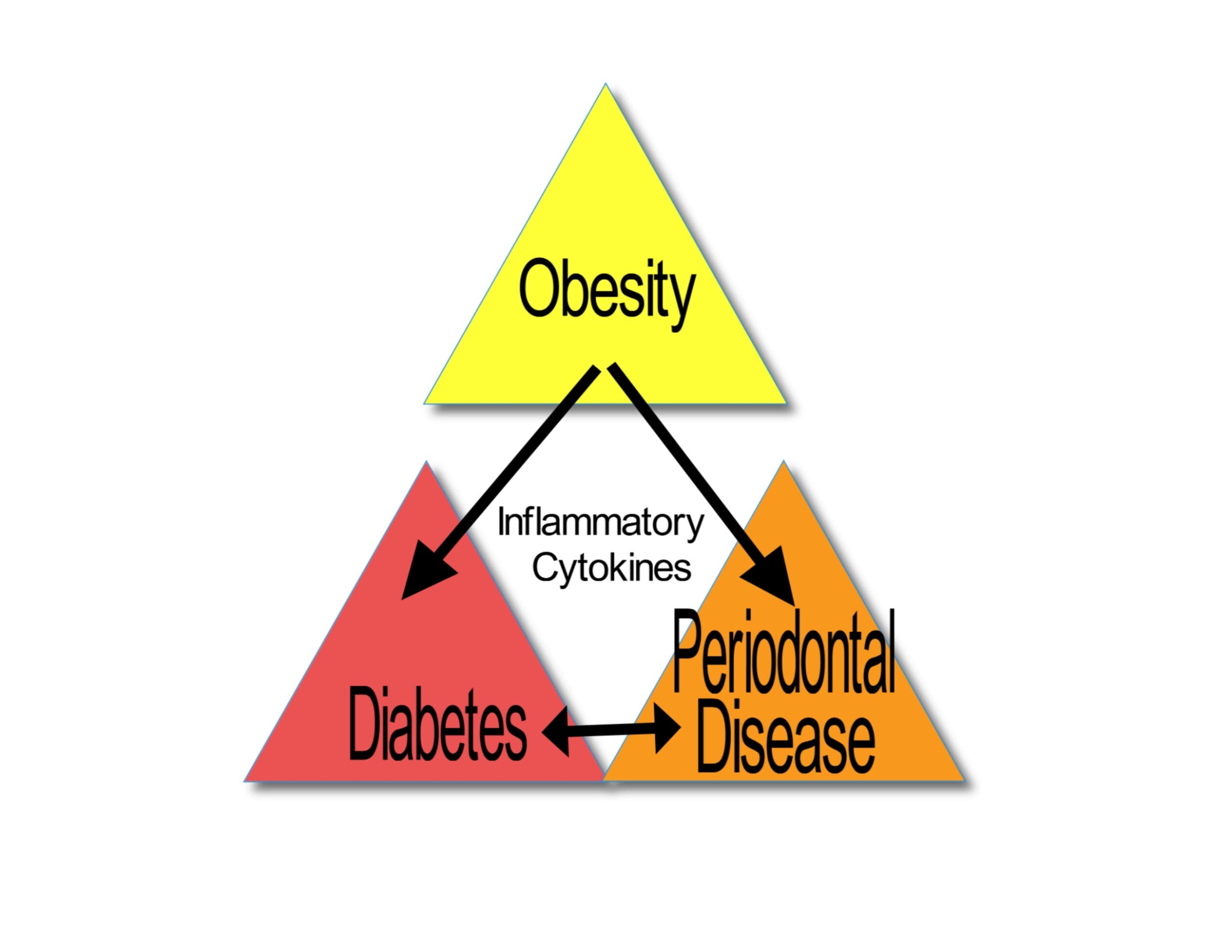
Figure 1 – It’s A Three-Way Street. Image courtesy of Nick Timko.How periodontitis affects diabetes ‒ The effect of periodontitis on diabetes is believed to result from the actions of the inflammatory response to periodontal pathogens in the periodontium (the term used to collectively label the gingiva, periodontal ligament, cementum, and alveolar bone).11 Some pathogens from infected gingiva leak into the bloodstream after normal chewing or brushing teeth. The body’s defense system is turned on, and the resulting pathogen-associated molecular patterns (PAMPs) can raise blood sugar.12,13 (PAMPs are molecules that activate the body’s immune response. A well-known PAMP is a lipopolysaccharide (LPS), which is found on the outer cell wall of gram-negative bacteria such as the major periodontal pathogen Porphyromonas gingivalis.)
How diabetes affects periodontitis ‒ The connection between diabetes and oral health issues is high blood sugar. Problems are more likely to develop when an individual’s blood sugar is poorly controlled. The chief problem with poor blood sugar control is that it weakens white blood cells that are the body’s primary defense against oral bacterial infections, the cause of periodontal disease.14 Diabetes also causes blood vessel changes. Excess blood sugar decreases blood vessel elasticity, which causes a narrowing of the vessel. This restricts blood flow, bringing about a reduced blood oxygen supply and giving rise to an increased likelihood of inflammation and infection in the gingiva and alveolar bone. If diabetes is poorly controlled, the higher blood sugar levels in the mouth fluids will help the bacteria that cause gum disease to grow and multiply.15
What is Diabetes?
Diabetes (or diabetes mellitus) is a chronic disease where the blood sugar (or blood glucose, a type of simple sugar) levels are too high. Diabetes comes from the Greek word diabainein, meaning “to pass through,” referring to increased urination. Mellitus comes from a Latin phrase meaning “sweetened with honey,” referring to sugar in the urine.) The pancreas produces the hormone insulin to help break down the sugars in the diet. Blood glucose is the main energy source for the body. If it can’t produce insulin (known as type 1 diabetes – an autoimmune reaction, where your body mistakenly attacks itself, stopping the pancreas from producing any insulin), or produces some, but not enough insulin (type 2 diabetes, where the body does not use what little insulin it produces effectively), the sugars in a diet increase to excessive levels in the blood. About 10% of diabetics are type 1, and 90% are type 2.
In addition, a type of diabetes known as gestational diabetes develops in pregnant women who never had diabetes until becoming pregnant. It usually disappears after the woman gives birth, but both baby and mother risk diabetic issues.
Classic symptoms of undiagnosed or uncontrolled diabetes include polyuria (frequent urination), polydipsia (excessive thirst), polyphagia (excessive hunger), weight loss, and a change in periodontal disease severity.
The most common complications associated with diabetes are heart disease (including stroke), foot issues (because diabetes reduces blood circulation), kidney disease, and problems with the eyes.
What is Periodontal Disease?
Periodontal (gum) disease is an infection of the gingiva and the bone that holds the teeth in place. It is a chronic inflammatory response to the accumulation of dental plaque. Plaque is composed of bacteria and other microorganisms in the mouth that form a sticky, colorless (or pale yellow) film on the teeth after eating and drinking.
This yellow film is called a biofilm, a community of microbes encased in a polymer matrix. The pathogenic bacteria within the biofilm acquire antibiotic resistance and communicate with each other by quorum sensing molecules. This organized biofilm ‒ the community of neighboring bacterial cells ‒ is able to survive better than the individual bacterial cells.
The pathogenic bacteria in plaque are seen as foreign invaders to the body, so the body triggers its first line of defense (innate immunity) and also calls up various enzymes that up-regulate cytokines. The important point is that even though the pathogenic bacteria are the cause of the disease, they do little direct damage. The immune response they trigger leads to inflammation, and it is the produced matrix metalloproteins (MMPs) enzymes) that destroy the collagen framework of the periodontal tissue.16
The risk factors for periodontal disease include smoking, poor home care, unresolved stress, other dental issues (such as missing or crooked teeth or rough restorations), weak immunity, or genetics. If you suffer from any combination of these, plaque will continue to grow, multiply and eventually harden into tartar (or dental calculus). The dental hygienist is trained in the best methods for removing plaque and calculus. At home, the patient needs to understand that these periodontal bacteria grow quite rapidly; they double in number every 4.8 hours!17 This means that if the patient only brushes once per day, they’ve allowed five doubling cycles to occur, whereas a twice a day brusher allowed only 2.5 doublings. That’s significant when you talk about some 20 billion bacteria in the human mouth (60 billion bacteria [with 2.5 doublings] vs. 120 billion [with five doublings])!
In its earliest stages, conventionally known as gingivitis, it affects only the gingiva, making them red, puffy, and inflamed. If it continues to be ignored, factors such as genetics, medicines, and inadequate oral home care cause it to grow beneath the gingival margin, where the older plaque has already migrated and turned into calculus. This porous, hardened calculus becomes a great breeding ground for the newer, more virulent (disease-causing) plaque that will begin to literally cause the supporting alveolar bone to be eaten away (see Figure 2).
Once you begin to lose this supportive bone, the teeth eventually loosen, and if left to continue, you will have lost so much bone that the tooth will literally fall out, even if the tooth has no decay. I’m sure that every hygienist has had a perio patient in their chair and literally had to hold a wobbly tooth in place to be able to clean that tooth for fear of accidentally removing it if they didn’t (see Figure 3).
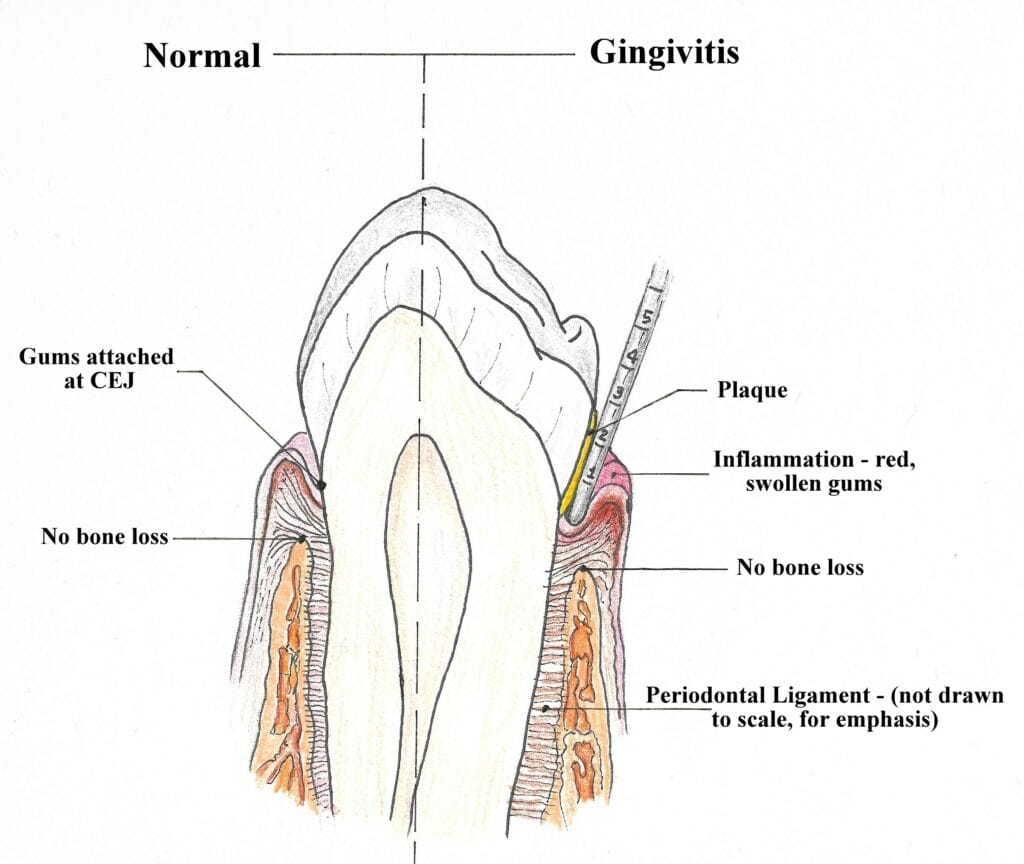
The best analogy I use for explaining to patients how a tooth is held in place in your mouth is to picture a trampoline. The trampoline itself is like a tooth, the springs that hold it to the frame are like the periodontal ligaments (collagenous bundles of connective tissue) that hold the tooth to the surrounding bone, and the frame that supports the trampoline and sits on the floor is like the alveolar bone that holds the tooth in place. Now, if you imagine the springs to be heavy-duty, rigid springs, the strength of these rigid springs is like the periodontal ligaments holding the tooth rigidly in place in the bone.
In reality, the width of the periodontal ligament averages about 0.25mm, and it narrows as you age. (It would take over 100 of them to equal one inch.) You seldom, if ever, actually feel the tooth move because it’s held so rigidly in place, but in reality, the tooth is floating via the periodontal ligaments rather than being fused to the bone in any way. If you lose enough of the connective tissue in the periodontal ligament (springs) through ongoing periodontal disease, the tooth will eventually loosen and fall out.
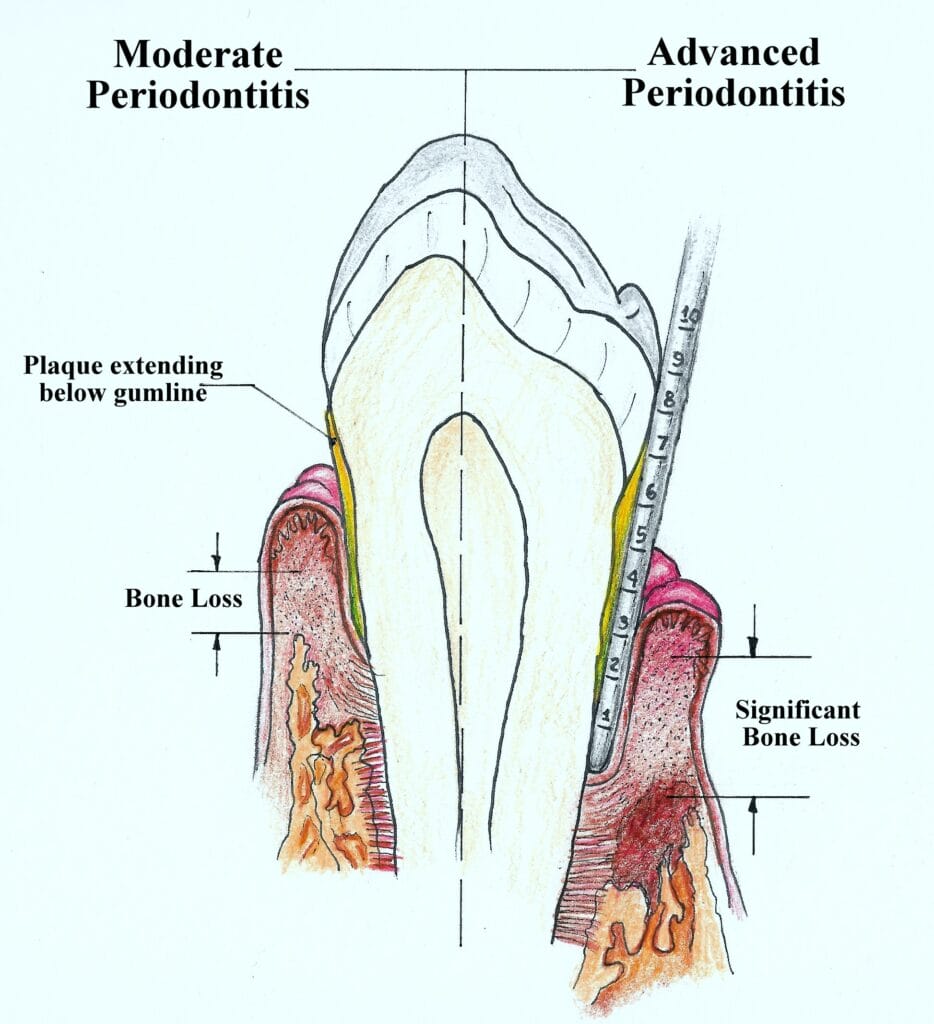
Gingivitis is reversible, and your dentist and dental hygienist can help you achieve that goal, but once it has progressed to what is commonly known as periodontitis, it is no longer reversible. The best we can hope for at that stage is to halt the progression of the disease so as to minimize any further loss of bone, tooth deterioration, and tooth loss.
Some symptoms of periodontal disease (depending upon how far it has progressed) include red, puffy gums, tartar buildup on teeth (calculus), persistent bad breath (halitosis), bleeding and/or purulent exudate (pus) oozing from the gingiva, pocket formation/increased probing depth noted by the hygienist, formation of furcations, and tooth mobility.
Conclusion
Periodontal disease, diabetes, and obesity are all worldwide epidemics. This means that most hygienists will see patients that have all three of these afflictions. Taking and updating a thorough health history, connecting with the patient to the point where they trust you and the advice you share with them, and then adequately treating the patient’s periodontal disease will help that patient in the best way possible with the one, two, or possibly three linked epidemic afflictions affecting their life.
Need CE? Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Vavrosky, K.D. (2019, February 11). Comprehensive Health History: Are You Doing A Thorough Review? Today’s RDH. Retrieved from https://www.todaysrdh.com/comprehensive-health-history-are-you-doing-a-thorough-review/
- Snyder, L. (2021, December 7). What Patients Need to Know About Periodontitis Links to Diabetes and Heart Disease. Today’s RDH. Retrieved from https://www.todaysrdh.com/patients-need-know-periodontitis-links-diabetes-heart-disease/
- Broom, D. (2020, December 14). The Silent Epidemic that is three times as deadly as COVID. World Economic Forum. Retrieved from https://www.weforum.org/agenda/2020/12/diabetes-silent-epidemic-world-health/
- Centers for Disease Control and Prevention. (2021, June 15). National Diabetes Statistics Report, 2020. Retrieved from https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Nocini, N., Lippi, G., Mattiuzzi, C. Periodontal Disease: the portrait of an epidemic. Journal of Public Health and Emergency. (2020, June, Vol.4). Retrieved from https://jphe.amegroups.com/article/view/5774/html
- Eke, P.I., Thornton-Evans, G.O., Genco, R.J., et al. Prevalence of Periodontitis in Adults in the United States; 2009 and 2010. CDCPeriodontal Disease Work Group. Journal of Dental Research. 2012;91:914-920. Retrieved from https://pubmed.ncbi.nim.nih.gov/22935673/
- Genco, R.J. The Three-Way Street. 2008. Scientific American publication Oral and Whole Body Health. pp 18-22.
- Obesity and Overweight. (2021, June 9). World Health Organization (WHO). Retrieved from https://who.int/news-room/fact-sheets/detail/obesity-and-overweight
- About Adult BMI. Retrieved from https://www.CDC.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- Popko, K., Gorska, A., Pyrzak, B., et al. Proinflammatory Cytokines IL-6 and TNF-α and the Development of Inflammation in Obese Subjects. European Journal of Medical research. (2010)15(SupplII):120-122. Retrieved from https://pubmed.ncbi.nim.nih.gov/21147638/
- Lamster, I.B., Laila, E., Borgnakke, W.S. et al. The Relationship Between Oral Health and Diabetes Mellitus. JADA. October 2008; Vol. 139
- Gum Disease Can Raise Your Blood Sugar Level. JADA. July 2013; 144(7). Retrieved from https://www.mouthhealthy.org/~/media/ADA/Publications/Files/FTDP_July2013_2.pdf?la=en
- Oindrila, P., Arora, P., Mayer, M. Inflammation in Periodontal Disease: Possible Link to Vascular Disease. Frontiers in Physiology. (2021, January 14). Retrieved from https://doi.org/10.3389/fphys.2020.609614
- Oral Health Problems and Diabetes. Cleveland Clinic Article. (2019, September 17). Retrieved from https://my.clevelandclinic.org/health/diseases/11263-oral-health-problems-and-diabetes
- Diabetes and Periodontal (Gum) Disease. Johns Hopkins Medicine. Retrieved from https://johnshopkinshealthcare.staywellsolutionsonline.com/RelatedItems/85,p00349
- Bussac, G., Periodontal Disease: Part 1 – Biological Mechanisms and Risk Factors. Practical Periodontics and Aesthetic Dentistry.-Feb. 1999;11(1) 53-56. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10218051/
- Landers, W. (2015, April 17). Periodontal Risk Assessment, Traditional vs. Microbiological Tests; SUNY-Broome Dental Hygiene Department Seminar powerpoint presentation slides; Binghamton, N.Y.; calculations from book by Dr. Walter Loesche, Dental Caries; A Treatable Infection, Univ. of Michigan (1987), (no longer in print).











