Social media has increased dental patients’ exposure to many trends, ranging from cleaning hacks to home health remedies. While some information can be helpful and improve a person’s quality of life, other trends may end up causing harm. Dental professionals need to stay up to date and prepared to best inform patients on the viability and safety of popular trends that may pertain to their oral health.
One of the most recent fads, mouth taping, claims to inhibit mouth breathing and improve oral health, snoring, sleep, and daily productivity. But is it safe or truly effective?
Breathing Through the Mouth
Dentistry has shifted from a treatment-centered approach focused on tooth restoration to a treatment and management-cooperative approach focused on improving, maintaining, and recovering oral function. Mouth breathing syndrome is a set of signs and symptoms that may be completely or incompletely present in people who, for various reasons, replace the correct nasal breathing pattern with an oral or mixed breathing pattern.1
Mouth breathing is a manifestation of poorly developed oral function and negatively influences the oral environment and craniofacial morphology in developing children. Mouth breathing can be induced in various situations, such as nasal congestion due to hypertrophic adenoids or allergic rhinitis, even in healthy individuals.1,2
Mouth breathing directly affects behavioral performance and dental health. During mouth breathing, malocclusion may occur, the intraoral space becomes dry, and saliva production is reduced.2 Mouth breathing during sleep is related to a lower intraoral pH in comparison with the pH associated with nasal breathing during sleep, indicating that mouth breathing could be a causal factor for dental erosion and caries.1
Prolonged mouth breathing can cause not only dental disease but also physical changes, such as an imbalance of craniofacial muscle activity and deformation of head posture produced by positional changes of the tongue, lips, and mandible.2 Mouth breathing during critical growth periods in children is associated with a higher tendency for clockwise rotation of the growing mandible, with a disproportionate increase in the anterior lower vertical facial height and decreased posterior facial height (see Figure 1). Overjet and the upper and lower incisor angles of mouth breathers may also be greater than those of nasal breathers.1
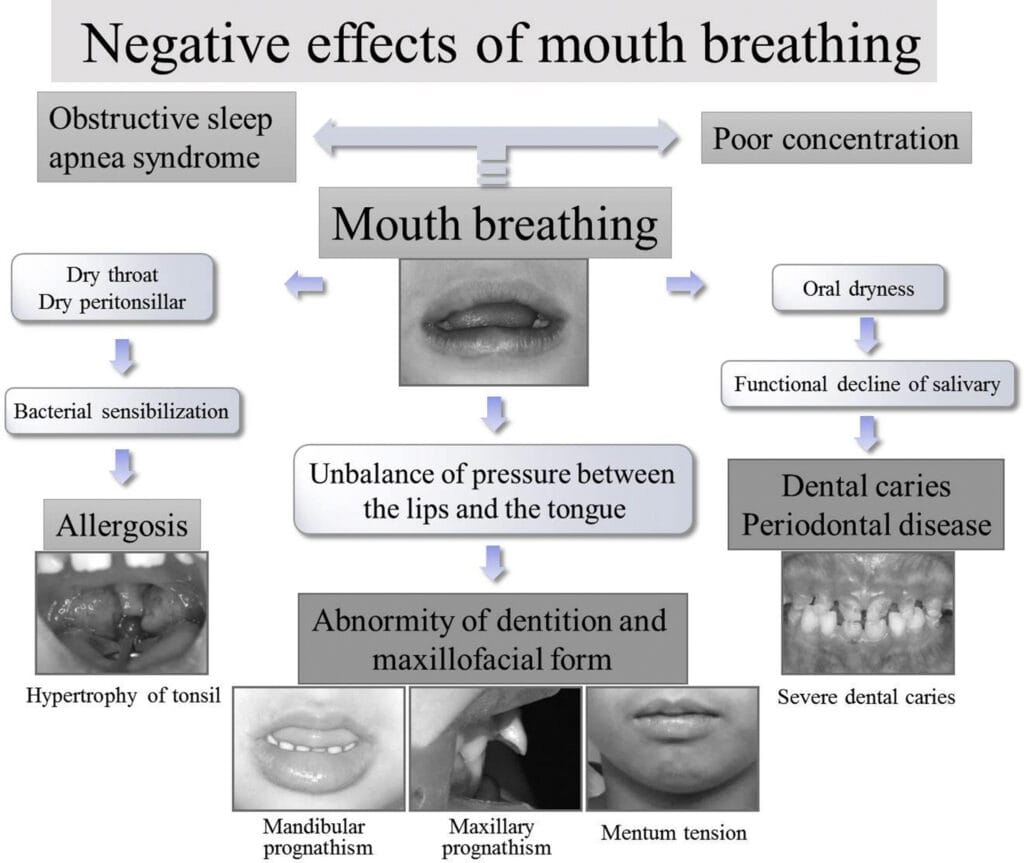
Figure courtesy Inada, et al.1
(CC BY-NC-ND 4.0)
One study aimed at investigating the effects of mouth breathing on cognitive function found that mouth breathing can affect pulmonary function and respiratory muscle activity. Failure to filter, humidify, and warm the inhaled air through mouth breathing may lead to decreased lung function and cognitive function due to lower oxygen saturation in the human brain. The study confirmed that the functional connection decreased significantly during a working task in mouth breathing rather than nasal breathing, causing a decline in working memory performance for specific cognitive tasks in children and olfactory memory tasks in healthy adults.2
Mouth breathing during sleep decreases the retropalatal and retroglossal areas via the posterior displacement of the soft palate and the inferior movement of the mandible, causing a reduction in the length of the upper-airway dilator muscles and may lead to snoring or obstructive sleep apnea.3
Snoring is the hoarse or harsh sound that occurs when air flows past relaxed tissues in the throat, causing the tissues to vibrate as a person breathes. The narrower the airway, the more forceful the airflow becomes, increasing tissue vibration and louder snoring. Anatomy of the mouth and sinuses, deviated nasal septum, alcohol consumption, weight, and allergies can contribute to snoring. Snoring is often associated with obstructive sleep apnea, although not all who snore have obstructive sleep apnea.4
There are several types of sleep apnea, but obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder. OSA occurs when throat muscles relax intermittently and block the airway, causing a person to stop and start breathing while asleep repeatedly. Symptoms include excessive daytime sleepiness, loud snoring, observed episodes of stopped breathing during sleep, and abrupt awakening accompanied by gasping or choking. Children with obstructive sleep apnea may do poorly in school and commonly have difficulty concentrating and behavior or attention problems.5
Risk factors for OSA are excess weight, older age, a narrowed airway, high blood pressure, chronic nasal congestion, smoking, diabetes, family history of OSA, and asthma associated with OSA.5
Research on Mouth Taping
Mouth taping is considered a home remedy to treat mouth breathing while sleeping and claims to improve health conditions related to oral health, allergies, snoring, and sleep apnea.6 The idea is to use skin-safe tape placed on the philtrum, spanning the upper and lower lips to seal the mouth during sleep to force nasal breathing.3,7
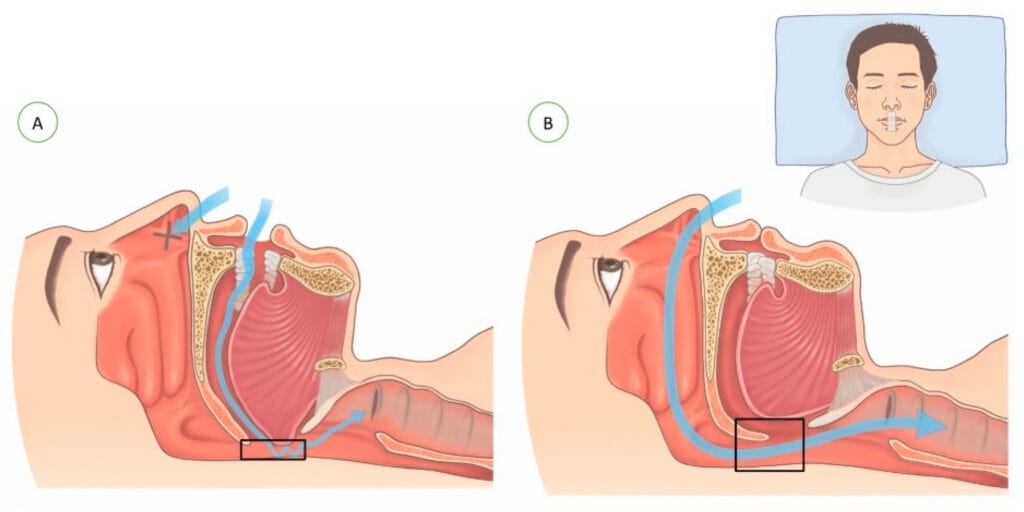
Figure courtesy Lee, et al.3
(CC BY 4.0)
Studies on mouth-taping benefits are currently limited and have varied results. In a randomized study of 51 participants, mouth taping was used in an attempt to promote the Buteyko nasal breathing technique to improve symptomatic asthma while asleep. However, no differences were found in morning peak expiratory flow or symptom score outcomes using mouth tape.8
Another study aimed at finding out if mouth puffing may be an indicator of obstructive sleep apnea found that mouth tape may be able to prevent patients with OSA from inhaling through the mouth but could not prevent patients from exhaling through the mouth.9
Conversely, in a 2022 study, 13 out of 20 participants showed “a good response” after one week of mouth taping. The apnea index (AI) measures a decrease in the airflow by 90% of baseline for at least 10 seconds, the hypopnea index (HI) measures the decrease in the airflow by 30% to 90% of baseline in addition to a > 3% reduction in oxygen saturation for at least 10 seconds per hour. Apnea/hypopnea index (AHI the sum of AI and HI per hour) and the snoring events per hour (SI) were reduced by nearly 50% after mouth taping during sleep in this study.3
It is important to note that this study had a small sample size of 20 people (19 men and one woman) with mild OSA. The researchers state there was no control group, so “no comparison could be made to determine whether there was a placebo effect.”3 Inclusion criteria for the study included those who could tolerate having their mouths taped, which may have led to more favorable results. Further limitations of this study are that it was a retrospective study with a short follow-up period; no long-term effects were evaluated. This study also used home sleep tests, which may underestimate the severity of OSA.3
A pilot study looked at treating OSA and habitual open-mouth breathing using porous oral patches. Porous oral patches (POP) consist of three layers: A silicone sheet, polyurethane foam, and polyurethane film.10
Subjective outcomes were assessed using the Epworth Sleepiness Scale (ESS) and visual analog scale of snoring (VAS). Objective outcomes were assessed using polysomnography and cephalometry of 30 participants. ESS and VAS before POP were 8.1 ± 1.5 and 7.5 ± 2.0, respectively, and after POP were 5.2 ± 1.6 and 2.4 ± 1.4, respectively (P < .05). Snoring intensity and median snoring index before POP were 49.1 ± 10.8 dB and 146.7 per hour before POP and 41.1 ± 7.8 dB and 40 per hour following POP use. Cephalometry revealed the retropalatal space and retrolingual space were 7.4 ± 1.6 mm and 6.8 ± 2.5 mm before POP and 8.6 ± 1.2 mm and 10.2 ± 1.8 mm following POP.10
The researchers suggest POP was a useful device for the treatment of patients with OSA and habitual open-mouth breathing.10
It’s important to note that a small sample size of 30 participants was studied, and the AHI became worse in one-third of the participants. This indicates that POP may not be suitable for all OSA patients and can make OSA symptoms worse.10
What Dental Professionals Should Advise
At this point, mouth taping is not recommended because there is not enough evidence to support the anecdotal benefits behind the trend.7 There are not enough studies to prove this technique treats any underlying health condition.
Kathryn Palmer, a sleep medicine specialist with Banner Health Colorado, believes mouth taping may be dangerous to those suffering from OSA because mouth breathing is a backup. She states risks include blocking airflow, worsening sleep apnea, skin irritation or allergic reaction to tape, or aspiration of stomach contents into the lungs if a patient vomits or has acid reflux that may lead to pneumonia or death.11
Mouth breathing treatments can be as simple as over-the-counter allergy medications or nasal strips to more invasive options such as a continuous positive airway pressure machine (CPAP), sleep studies, or surgery.7
It is estimated that 85% of patients with clinically significant and treatable OSA have never been diagnosed.9 Dental professionals who notice signs and symptoms of mouth breathing in patients should recommend that they reach out to their primary care provider to directly address the underlying causes of their condition or be referred to a sleep medicine physician, ENT, pulmonologist, and/or orofacial myofunctional therapist.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Inada, E., Saitoh, I., Kaihara, Y., Yamasaki, Y. Factors Related to Mouth-breathing Syndrome and the Influence of an Incompetent Lip Seal on Facial Soft Tissue Form in Children. Pediatric Dental Journal. 2021; 31(1): 1-10. https://doi.org/10.1016/j.pdj.2020.10.002
- Jung, J.Y., Kang, C.K. Investigation on the Effect of Oral Breathing on Cognitive Activity Using Functional Brain Imaging. Healthcare. 2021; 9(6): 645. https://doi.org/10.3390/healthcare9060645
- Lee, Y.C., Lu, C.T., Cheng, W.N., Li, H.Y. The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare. 2022; 10(9): 1755. https://doi.org/10.3390/healthcare10091755
- Mayo Clinic Staff. (2017, December 22). Snoring. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/snoring/symptoms-causes/syc-20377694
- Mayo Clinic Staff. (2023, July 14). Obstructive Sleep Apnea. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/symptoms-causes/syc-20352090
- Cherney, K. (2024, September 18). Mouth Taping: Does It Treat Snoring or Sleep Apnea? Healthline. https://www.healthline.com/health/taping-mouth
- Mouth Taping: Is It Safe? (2022, September 7). Cleveland Clinic. https://health.clevelandclinic.org/mouth-taping/
- Cooper, S., Oborne, J., Harrison, T., Tattersfield, A. Effect of Mouth Taping at Night on Asthma Control – A Randomised Single-blind Crossover Study. Respiratory Medicine. 2009; 103(6): 813-819. https://doi.org/10.1016/j.rmed.2009.02.003
- Jau, J.Y., Kuo, T.B.J., Li, L.P.H., et al. Mouth Puffing Phenomena of Patients With Obstructive Sleep Apnea When Mouth-Taped: Device’s Efficacy Confirmed With Physical Video Observation. Sleep and Breathing. 2022; 27: 153-164. https://doi.org/10.1007/s11325-022-02588-0
- Huang, T.W., Young, T.H. Novel Porous Oral Patches for Patients with Mild Obstructive Sleep Apnea and Mouth Breathing. Otolaryngology-Head and Neck Surgery. 2015; 152(2): 369-373. https://doi.org/10.1177/0194599814559383
- Thurrott, S. (2023, March 6). Can Mouth Taping Help You Sleep Better? Banner Health. https://www.bannerhealth.com/healthcareblog/teach-me/why-you-should-never-tape-your-mouth-closed-when-you-sleep