
Recently, I encountered two situations that inspired this article. I came across a periapical radiograph of a new patient with a radiolucency, presenting as a well-defined lesion distal to an extracted mandibular second molar. The extraction was done about six months prior.
Another incident was when a new patient with a unilocular lesion at the apex of #29 was referred to an endodontist. The endodontist performed root canal treatment. However, the lesion was still present radiographically months after the treatment without changes in appearance and size.
Cyst vs. Abscess
Differentiating between a cyst and an abscess can sometimes be challenging. Knowing the common cysts, their etiology, and specific features minimize misdiagnosis.
A cyst is a sac lined with epithelium tissue and enclosed by connective tissue, which can be filled with, for example, fluid, hair, or blood.1 The types of cysts are determined by their origin and location.
An abscess usually happens as a result of:2,3
- Gross decay that is left untreated
- Secondary to any dental decay
- Trauma to a tooth
- Poor oral hygiene
- Initial root canal therapy
The severity of the abscess depends on the level of virulence of the bacteria (mostly anaerobes), the individual’s oral hygiene, and immune response.2,3 These bacteria can reach the tooth via any opening, such as failed restorations, trauma to the soft and hard tissue of the tooth, and fractures.2 The bacteria can cause infection within the tooth, move towards the tooth canal, and then accumulate at the apices of the tooth.2,3
Accumulation of bacteria leads to infection, which may cause pain, fistula, bad taste in the mouth, and severe problems such as septicemia, cavernous sinus thrombosis, brain abscess, shock, and occasionally death if left untreated.3 (see Image 1)
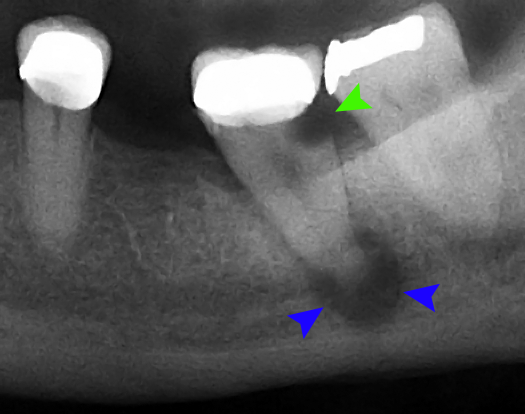
Image courtesy Coronation Dental Specialty Group (CC BY 3.0 via Wikimedia Commons)
Mistaken for an Abscess
Sometimes, it is hard to differentiate a cyst from an abscess. Knowing the common location of certain cysts and their appearance may help to minimize misdiagnosing. Some cysts that are potentially problematic when making a definitive diagnosis are nasopalatine duct cyst, central giant cell granuloma, periapical cyst, lateral periodontal cyst, dentigerous cyst, and odontogenic keratocyst, as they can resemble an abscess.1,2,4-6
Nasopalatine duct cyst: This occurs around the nasopalatine canal, and it has a heart shape and a well-defined appearance. Pain may or may not be present, and treatment includes cyst removal. Radiographically, a heart shape (or sometimes a tear shape), unilocular radiolucency is present at the apex of 8 and 9.1 (see Images 2 and 3)
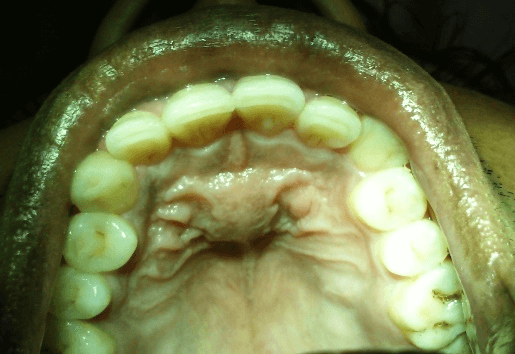
Image courtesy Patil, R., et al.7 (CC BY 4.0 DEED)
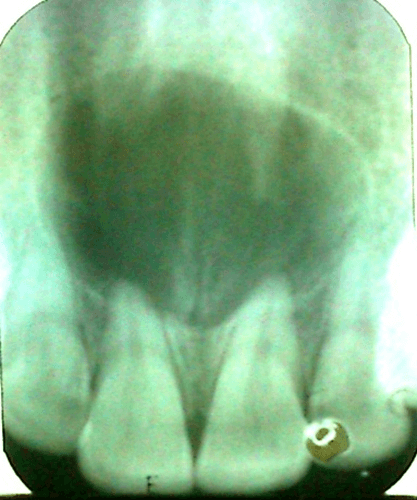
Image courtesy Patil, R., et al.7 (CC BY 4.0 DEED)
Central giant cell granuloma: It appears as a multilocular lesion on a radiograph and is bigger than an abscess in size and shape; therefore, it should not be mistaken for an abscess.1 (see Image 4)

Image courtesy ASEDATC (CC BY-SA 4.0 via Wikimedia Commons)
Periapical cyst: Also known as a radicular cyst, this is the most common oral cyst that occurs around the apices of a nonvital tooth and mostly around anterior maxillary teeth.1,2 It is mostly asymptomatic and radiographically appears as a well-defined, unilocular radiolucency at the apex of the tooth.1
If the cyst is not treated properly, it can lead to a residual cyst.1,4 The treatment consists of tooth and cyst removal. However, if it is mistaken for a dental abscess, the cyst stays in the area after the root canal treatment.1 To see radiographic images of a radicular cyst, click here.
Lateral periodontal cyst: This cyst is unilocular, radiolucent, well-defined, and lateral to the tooth, which usually occurs around mandibular premolars and canines, even though it can be found around maxillary premolars and canines as well. This cyst is asymptomatic and occurs in vital teeth, so the patient may not be aware of its presence. The treatment is excisional with an excellent prognosis.1 (see Image 5)
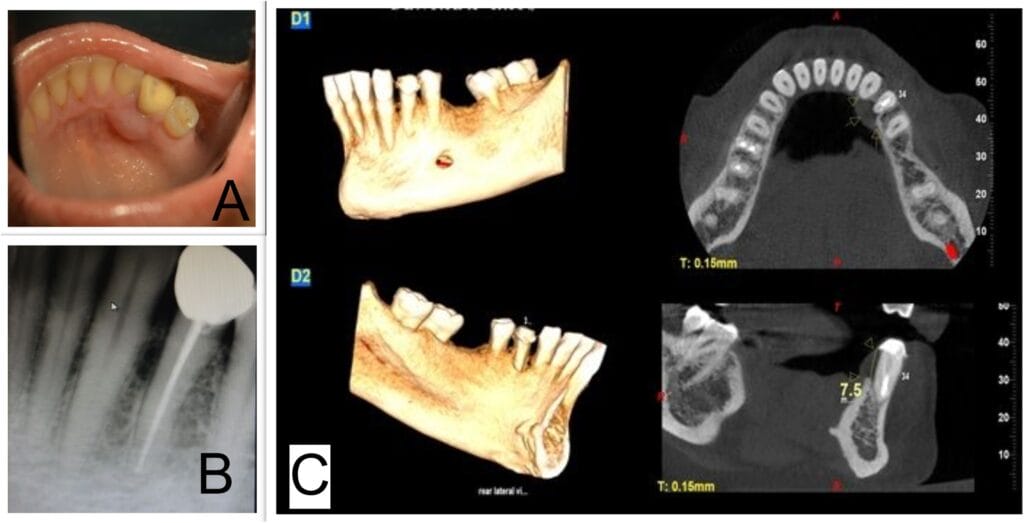
Image courtesy Ramesh, R., et al.8 (CC BY 4.0 DEED)
Dentigerous cyst: Generally asymptomatic, this cyst is the second most common cyst occurring around the crown of an impacted tooth, unerupted tooth, supernumerary tooth, or odontoma. Therefore, it is not unexpected to see this cyst around the impacted third molars of young adults. This cyst appears well-circumscribed on a radiograph. To treat this cyst, tooth extraction and excisional removal of the cyst proved to have an excellent prognosis, although the area must be evaluated regularly for ameloblastoma.1 (see Image 6)

Image courtesy JawCyst.jpg: Coronation Dental Specialty Group [1]derivative work: Jbarta and Mikael Häggström (CC BY 3.0 via Wikimedia Commons)
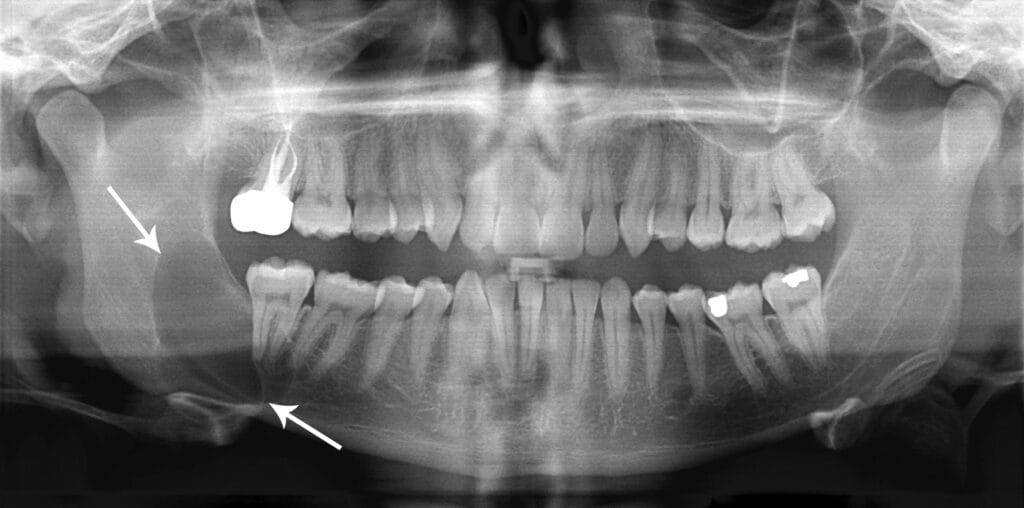
Courtesy Coronation Dental Specialty Group (CC BY 3.0 via Wikimedia Commons)
The following table helps with differentiating these common cysts that can be mistaken for an abscess.
| Cyst | Radiographic Appearance | Common Location | Pain or No Pain | Unique Specification |
| Nasopalatine duct cyst | Heart-shape unilocular | Nasopalatine canal, around teeth 8 and 9 | May or may not be present | Heart-shaped |
| Periapical cyst (radicular cyst) | Unilocular radiolucency at the apex | Maxillary anterior, although can happen around all the apices of all the teeth | Asymptomatic | The most common cyst, occurs around nonvital teeth |
| Lateral periodontal cyst
|
Unilocular, well-defined, lateral to the tooth | Favors mandibular premolars and canines | Asymptomatic | Occurs around vital teeth |
| Dentigerous cyst | Well circumscribed | Associated with impacted teeth, unerupted teeth, supernumerary teeth, or odontoma | Asymptomatic | The 2nd most common cyst |
| Odontogenic keratocyst (OKC) | Unilocular or multilocular | Three times higher in mandibular teeth than maxillary teeth | Pain may or may not be present | The 3rd most common cyst, external root resorption may be present |
In Closing
Differentiating between a cyst and an abscess can sometimes be challenging. Knowing the common cysts, their etiology, and specific features minimize misdiagnosis. If in doubt, it is better to refer patients to an endodontist or an oral surgeon for further evaluation.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- DeLong, L., Burkhart, N.W. (2012). Radiolucent Lesions. In General and Oral Pathology for the Dental Hygienist (2nd ed., pp. 517-548). Jones and Bartlett Learning.
- Sanders, J.L., Houck, R.C. (2023, February 20). Dental Abscess. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493149/
- Shweta, S., Prakash, K. Dental Abscess: A Microbiological Review. Dental Research Journal. 2022; 10(5): 585-591. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858730/
- Gnepp, D.R. (2021). Odontogenic Cysts and Tumors. In V.I. Woo, A.C. Chi, B.W. Neville, Gnepp’s Diagnostic Surgical Pathology of the Head and Neck (3rd ed., pp. 827-880). Elsevier. https://doi.org/10.1016/B978-0-323-53114-6.00010-9
- Borghesi, A., Nardi, C., Giannitto, C., et al. Odontogenic Keratocyst: Imaging Features of a Benign Lesion with an Aggressive Behaviour. Insights into Imaging. 2018; 9(5): 883-897. https://doi.org/10.1007/s13244-018-0644-z
- Harmon, M., Arrigan, M., Toner, M., O’Keeffe, S.A. A Radiological Approach to Benign and Malignant Lesions of the Mandible. Clinal Radiology. 2015; 70(4): 335-350. https://doi.org/10.1016/j.crad.2014.10.011
- Patil, R., Patil, A., Tupsakhare, S., et al. Nasopalatine Duct Cyst: A Case Report and Review of Literature. Global Surgery Case Reports. 2020; 2(2). https://www.sciencerepository.org/nasopalatine-duct-cyst-a-case-report-and-review-of-literature_GSCR-2020-2-104#_
- Ramesh, R., Sadasivan, A. Lateral Periodontal Cyst – A Diagnostic Dilemma: Report of a Rare Case with CBCT and Histological Findings. International Journal of Surgery Case Reports. 2020; 75: 454-457. https://www.sciencedirect.com/science/article/pii/S2210261220307628
- Dave, M., Clark, L., Grindrod, M., et al. Adapting Treatment Approaches for Dentigerous Cysts in Pediatric and Adult Patients: A Case Series. Oral Surgery. 2019; 14(3): 277-284. https://doi.org/10.1111/ors.12575











