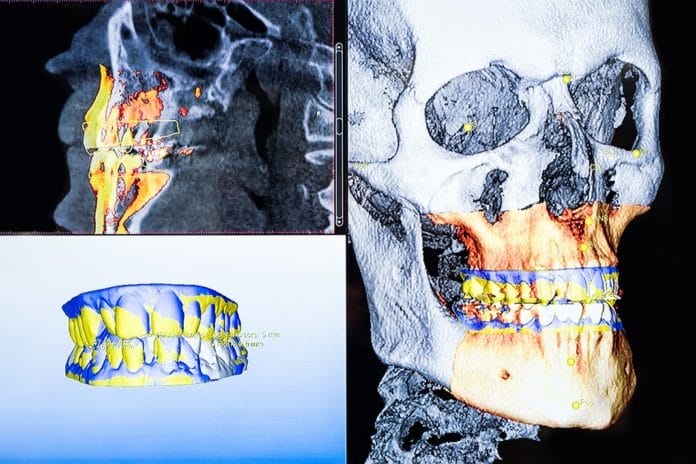
The potential for three-dimensional imaging in dentistry is widespread. Hygienists use two-dimensional images on a daily basis, but they do not provide the amount of detail that the three-dimensional counterpart does.
According to one source, “In two-dimensional imaging, evaluation of bone craters, lamina dura, and periodontal bone level is limited by projection geometry and superpositions of adjacent anatomical structures.” Two-dimensional imaging can also distort certain anatomical features, and those distortions are eliminated by three-dimensional imaging.1 While three-dimensional imaging can be utilized in all areas of dentistry, some of the most common usages are in three areas of specialization − periodontics, endodontics, and orthodontics.
Applications in Perio
In the practice of periodontics, three-dimensional imaging provides invaluable data to clinicians. It can help determine the amount and quality of bone prior to treatment, but it can also be used to evaluate bone levels before and after regeneration procedures.2
Being able to closely evaluate the quality and quantity of bone is imperative when determining the best course of periodontal treatment for patients. Is the patient a candidate for osseous surgery? Bone grafting? Implants? This can all be determined by utilizing three-dimensional imaging along with clinical data.
In regard to dental implants, anatomical features should be considered prior to placement. The location of the maxillary sinus and mandibular nerves are two of the most common limitations to whether or not a patient is a candidate for implant treatment. If the maxillary sinus is too low, the patient may need a sinus lift prior to implant therapy. If the mandibular nerve sits too high, it may prevent a patient from being a candidate altogether.
The clinician can utilize the three-dimensional imaging software to virtually place the implants, which allows them to determine the size/type of implant and exact location prior to the day of the procedure.3 This helps cut down on surgical time and produce predictable outcomes as well as improved patient experience. Three-dimensional images utilized today are so accurate that their measurements are almost equivalent to the in-mouth measurements taken the day of surgical procedures.4
Endo Views
There are clinical complications that cannot be detected on two-dimensional imaging but can be identified on their three-dimensional counterparts. Some examples of this include accessory canals, vertical root fractures, root resorption, and small periapical lesions.6 All of these insights can be extremely helpful in the practice of endodontics.
A vertical root fracture can be very difficult to diagnose clinically while utilizing two-dimensional images. But due to its high sensitivity, a three-dimensional image is much more likely to reveal this than its two-dimensional counterpart.7
As hygienists, we can greatly appreciate this because for some of our patients’ it is very difficult for them to pinpoint where the symptoms are arising from. How many times have you had a patient in your chair who can’t locate if their toothache is coming from the maxillary or mandibular region, or anterior or posterior? Having a detailed image that can help locate the source of a patient’s pain and discomfort is invaluable.
Ortho Candidates
There are many clinical determining factors as to whether or not a patient is a candidate for orthodontics; bone quality, airways, TMJ disorders, tooth/root positions, and skeletal patterns are just a few. Three-dimensional images can evaluate all of these in a much more detailed manner than a two-dimensional image can.
An example of this in everyday practice would be to use the images to aid in treatment planning for orthognathic surgery. The image can be used to evaluate skeletal growth patterns and discrepancies.8,9 It can also be used to determine eruption times and patterns, malposition of teeth, and potential airway obstructions.9,10
In my office, it is our practice to have patients sign a consent form prior to exposing a three-dimensional film, which can prompt them to question the safety of this type of imaging. This can be a great opportunity for patient education. One three-dimensional film can decrease the amount of radiation the patient is exposed to because the clinician does not have to take multiple two-dimensional films to get the information they need.9 As with any dental procedure, the benefit to the patient should always outweigh any potential risks.4
I have found that patients greatly appreciate it when they are shown the three-dimensional image after exposure, and the clinical findings are explained to them. This helps patients to understand recommended treatment better and feel as though they are included in their care.
Now Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Acar, B., Kamburoğlu, K. Use of Cone Beam Computed Tomography in Periodontology. World J Radiol. 2014; 6(5): 139-47. DOI: 10.4329/wjr.v6.i5.139.
- Vandenberghe, B., Jacobs, R., Yang, J. Detection of Periodontal Bone Loss Using Digital Intraoral and Cone Beam Computed Tomography Images: An In Vitro Assessment of Bony and/or Infrabony Defects. Dentomaxillofac Radiol.2008; 37(5): 252-60. DOI: 10.1259/dmfr/57711133.
- Mol, A., Balasundaram, A. In Vitro Cone Beam Computed Tomography Imaging of Periodontal Bone. Dentomaxillofac Radiol.2008; 37(6): 319-24. DOI: 10.1259/dmfr/26475758.
- Klokkevold, P. Cone Beam Computed Tomography for the Dental Implant Patient. J Calif Dent Assoc.2015; 43(9): 521-30.
- Grimard, B.A., Hoidal, M.J., Mills, M.P., Mellonig, J.T., Nummikoski, P.V., Mealey, B.L. Comparison of Clinical, Periapical Radiograph, and Cone-Beam Volume Tomography Measurement Techniques for Assessing Bone Level Changes Following Regenerative Periodontal Therapy. Journal of Periodontology. 2009; 80(1): 48-55.
- Fernández, R., Cadavid, D., Zapata, S.M., Álvarez, L.G., Restrepo, F.A. Impact of Three Radiographic Methods in the Outcome of Nonsurgical Endodontic Treatment: A Five-Year Follow-up. Journal of Endodontics. 2013; 39(9): 1097–1103.
- Chang, E., Lam, E., Shah, P., Azarpazhooh, A. Cone-beam Computed Tomography for Detecting Vertical Root Fractures in Endodontically Treated Teeth: A Systematic Review. Journal of Endodontics. 2016; 42(2): 177–185.
- Mallya, S.M. Evidence and Professional Guidelines for Appropriate Use of Cone Beam Computed Tomography. J Calif Dent Assoc.2015; 43(9): 512-20.
- Harrell, W.E. Jr. Three-dimensional Diagnosis and Treatment Planning: The Use of 3D Facial Imaging and 3D Cone Beam CT in Orthodontics and Dentistry. American Dental Practice. July/August 2007.
- Hodges, R.J., Atchison, K.A., White, S.C. Impact of Cone-beam Computed Tomography on Orthodontic Diagnosis and Treatment Planning. Am J Orthod Dentofacial Orthop.2013; 143(5): 665-74. DOI: 10.1016/j.ajodo.2012.12.011.