Healthy kidneys filter out metabolic wastes from our blood, which then pass through the urine, but renal failure patients may need the help of medical procedures, like hemodialysis, to remove this toxic buildup. Unfortunately, hemodialysis is also linked to higher rates of periodontal disease. A recent study from Egypt looked at the periodontal health of end-stage renal failure patients on hemodialysis and compared their oral health data to kidney failure biomarkers in order to elucidate potential relationships between the two.
Background on Oral Health and Kidneys
Patients with both kidney disease and periodontal disease often have other complications, like diabetes or high blood pressure. Socioeconomic and mental health factors may also play a role, potentially causing a patient to neglect their dental hygiene. Plus, both conditions are associated with inflammation, like chronic systemic inflammatory disease in renal failure patients, as well as periodontal inflammation. With increasing inflammatory levels, both conditions may worsen.
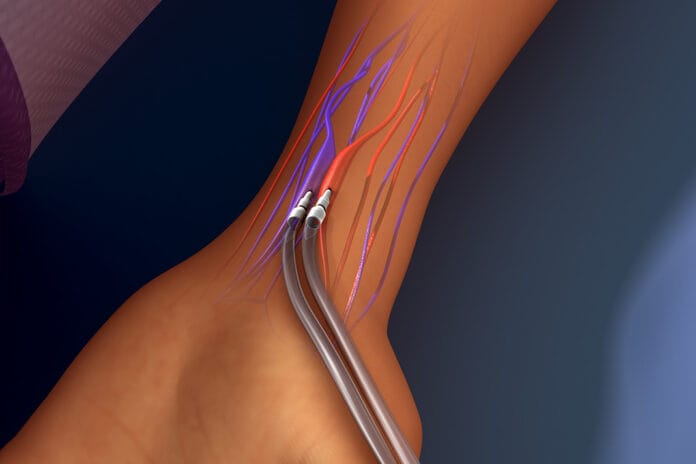
Hemodialysis patients often take various medications, like anticoagulants, that may affect oral health since blood thinners often cause increased bleeding on probing. Additionally, kidney disease usually leads to salivary changes, higher urea levels, and bone changes, further complicating oral health conditions.
The Study
This study included 263 patients on hemodialysis, 165 male and 98 female, from three dialysis centers in Egypt. All participants received an oral exam to evaluate and grade their oral health status, including, but not limited to, their plaque index, gingival index, clinical attachment level, and probing pocket depth.
Medical records and patient interviews provided further insight, like the length of time on hemodialysis, serum creatinine levels, blood urea levels, and whether these patients had other medical conditions. All data underwent statistical analysis.
Results
Findings show that 85.6% of these end-stage renal failure patients on hemodialysis had periodontal disease, and 14.4% had gingivitis. Of the 225 patients with periodontitis, 23.1% had stage II, 41.8% had stage III, and 35.1% had stage IV, making stage III periodontitis the most common.
From their medical history, the most prevalent diseases were hypertension (50.1%) and diabetes (21.5%), a finding in agreement with earlier studies. Additionally, patients in this study also had a history of Hepatitis C (16.5%), secondary hyperparathyroidism (5.5%), idiopathic renal disease (3.9%), and heart conditions (2.4%). A statistical analysis found a direct relationship between age, the length of time on hemodialysis, and the severity of periodontal disease.
Researchers also compared the patient’s recent blood urea and serum creatinine levels to their oral health data and found a few interesting associations. For one, with increasing age and higher blood urea levels, periodontal disease severity also increased. There was also a positive correlation between blood urea levels with plaque index, bleeding on probing, and clinical attachment level. Additionally, there was a positive correlation between serum creatinine levels and both probing pocket depth and clinical attachment level.
This study provides insight into potential links between periodontal disease and kidney function biomarkers. However, there are some limitations, like the absence of a control group, and lack of follow-up appointments, since this was a cross-sectional study. Further studies are recommended.
Some Patient Care Key Points
End-stage renal failure patients experience higher rates of periodontal disease, and for us dental hygienists, this study provides a few key points. Certain factors may play a role in the oral health status of hemodialysis patients, like age, the length of time on hemodialysis, or comorbidities. For example, hemodialysis patients with secondary hyperparathyroidism may experience jawbone complications, potentially leading to bone loss. Another interesting note from this study was the lack of gingival inflammation in pale gums, even with plaque and bleeding on probing. A previous study found that L-carnitine supplements, common in hemodialysis patients, may suppress inflammation, thus potentially hiding signs of gingival inflammation.
Receiving adequate dental care is very important for end-stage renal failure patients. Periodontitis worsens from a weakened immune system, as well as increasing levels of bacteria, and hence, leads to more inflammation. This compounding cycle may negatively affect both hemodialysis outcomes as well as oral health outcomes. Communication between the oral health team, nephrologists, and other healthcare professionals may greatly improve the patient’s quality of life.