While browsing social media, I recently stumbled upon a post on a dental hygiene page of an individual complaining about pain within the lateral aspect of her thumb. This particular post drew my attention since I have pain in the same area. Curious about other hygienists’ advice and responses, I scoured the comment section to find that many gave the same response that I suspected was the problem: De Quervain’s tenosynovitis.
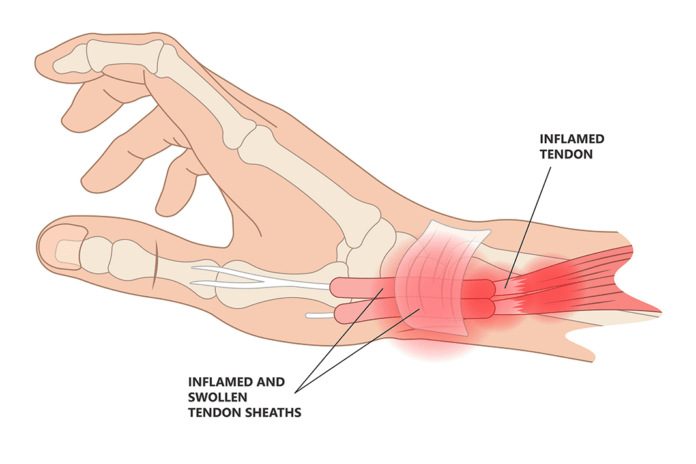
De Quervain’s tenosynovitis is swelling of the tendons that run along the thumb side of the wrist and attach to the base of the thumb.1 This condition occurs when the tendons that run from the wrist to the thumb are constricted by the sheath that encircles them.1
Two main tendons arise from the forearm and run to the thumb, assisting in creating movements. The abductor pollicis longus (APL) assists in bringing the thumb out away from the index finger. The extensor pollicis brevis (EPB) assists in straightening the joints of the thumb.1
Tendons are rope-like fibers that attach muscle to bone. A thin, slippery tissue called synovium allows the tendons to slide easily within the sheath that surrounds them. When swelling occurs within the tendon, it no longer fits properly inside the sheath, creating pain and irritation at the site. With repetitive wrist motions, specifically, motions requiring thumb radial abduction and simultaneous extension and radial wrist deviation, a thickening of the tendon sheath creates an entrapment of the tendons.2
De Quervain’s is named after a Swiss surgeon, Fritz de Quervain, who first described this condition in 1895.2 He speculated that it is an occupational disease augmented through industrial expansion and the increased demand for repetitive wrist motions.3
However, over the course of several decades, studies implicate that the etiology comes from more than just repetitive wrist motions. Multiple studies reveal striking amounts of mucinous and myxoid degeneration within the synovium of those afflicted with De Quervain’s. This indicates that the etiology of De Quervain’s may be related to specific inflammatory markers and genetic makeup in addition to repetitive motions.3
Those who are more at risk for De Quervain’s include:2,4
- Individuals with job tasks that involve repetitive movements of the hand and wrist
- New mothers or childcare workers
- Those with a previous history of arthritis
- Women and those ages 40 or older
De Quervain’s Tenosynovitis Signs and Symptoms
Those with De Quervain’s will notice pain or tenderness in the radial aspect of the wrist and pain upon resisted thumb extension.4 Crepitus of the tendons moving through the sheath may also be present.1
Tasks such as opening jars and squeezing or grasping objects may be challenging. Swelling, as well as difficulty moving the thumb, are also symptoms of De Quervain’s.1,5
Diagnosis and Treatment
Diagnosis is based on a clinical inspection with the Finkelstein test. In this test, the thumb is placed flat against the palm of the hand. A fist is made to encircle the thumb while pulling the thumb downward. If pain is felt in the radial wrist, De Quervain’s is likely the diagnosis. Radiographs may also be taken to rule out any arthritis within the joint.2
The treatment for de Quervain’s is rather simple, and the condition is often temporary and may resolve on its own. For those with persistent symptoms, corticosteroid injections, splinting, physical therapy, and systemic NSAIDS can all help alleviate and reduce inflammation.5
Splinting requires wearing a brace for four weeks to prevent the movement of the thumb, thus decreasing agitation.5 However, splinting may be difficult for dental professionals as grasping instruments requires the use of the thumb, something a splint prohibits. One to two corticosteroid injections in the tendon sheath have been reported to provide a 50% reduction after the first injection and an additional 40% to 45% after the second injection.2
Non-thermal therapeutic ultrasound therapy is another form of nonsurgical treatment that can be attempted to help alleviate symptoms by reducing inflammation and regenerating tissue. Ultrasound therapy is often performed under a physical therapist’s care and is sometimes used in conjunction with dexamethasone. Dexamethasone is a corticosteroid gel that is applied to the wrist and penetrated into the tendon with ultrasound therapy.3,6
If symptoms are not alleviated, surgery may be necessary to obtain relief. Surgical relief of the first extensor compartment is performed by a small incision. The nerves and veins are identified and protected first, then the sheath is partially resected. The tendons will be examined and evaluated to rule out any anatomical variations.3
Post-surgery, the thumb and wrist will be splinted for at least 10 to 14 days, followed by weeks of active range-of-motion exercises, scar/edema management, and strengthening exercises.3 In one study, complete pain relief was reported in 95% of the patients who underwent surgical treatment.7
If the condition is not treated, too much pressure on the tendon can permanently limit the range of motion, or rupturing of the tendon sheath is possible.8
Prevention
Sadly, there is not much to be done on the prevention side of this condition. Naturally, to reduce fatigue and unnecessary hand strokes, dental hygienists should ensure their instruments are sharpened frequently. Dulled instruments require more effort and time to remove calculus. Though an older study, it was concluded that a dental instrument typically begins to dull or show wear with beveling after just 15 strokes.9 Dental hygienists should also utilize ultrasonic scalers to help reduce hand fatigue.
My Story
When my twin boys were still infants, I was plagued with pain in my radial wrist upon lifting my children or simply a jug of milk. Strangely enough, I do not recall having any issues during clinical work. After a visit to the orthopedic clinic, I was diagnosed with De Quervain’s and given a corticosteroid injection and a splint. My pain completely resolved after this visit.
Fast forward nearly 12 years later, and my symptoms have returned. I tried wearing my splint more diligently as I had retained the habit of not wearing it at all. The pain became increasingly nagging and was affecting my work. I made an appointment with the same orthopedic group and was again given an injection.
For six months, I was pain-free. However, in December 2022, my symptoms slowly began to creep back in. I returned to my orthopedic group and, this time made sure I saw the hand specialist. He agreed with my previous diagnosis from years ago after reviewing radiographs of my hand and wrist. He gave me a second injection and discussed my options since the previous injection did not last very long.
Unfortunately, this injection did nothing more than dull the symptoms. Practicing clinically has become challenging. I wear my splint between patients but must remove it to treat patients. I also have to be careful about my patient load. When absolutely necessary, I take NSAIDS and use a prescription steroid-based cream to help with the discomfort, which seems to be more often lately. I also did several physical therapy visits where ultrasound therapy and ice massage were used to help with pain management. However, those visits began agitating my issue further, and I had to cease the treatment.
Currently, I have a consultation with a hand specialist for surgery that I hope to have prior to the year’s end. Hopefully, by the time some of you read this, I will be on the mend and pain-free.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- De Quervain’s Tenosynovitis. (n.d.). American Academy of Orthopedic Surgeons. https://orthoinfo.aaos.org/en/diseases–conditions/de-quervains-tendinosis/
- Satteson, E., Tannan, S.C. (2022, September 19). De Quervain Tenosynovitis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK442005/
- Fakoya, AOJ., Tarzian, M., Sabater, EL., et al. De Quervain’s Disease: A Discourse on Etiology, Diagnosis, and Treatment. Cureus. 2023; 15(4): e38079. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10208847/
- Oosting, K., Krenselewski, B., Dolislager, C. Effective Conservative Treatments for de Quervain’s Tenosynovitis: A Retrospective Outcome Study. Hand and Upper Extremity. 2013; 4. https://scholarworks.gvsu.edu/cgi/viewcontent.cgi?article=1003&context=ot_hand
- Knight, J. (n.d.). Mommy Thumb – de Quervain’s Stenosing Tenosynovitis. Hand and Wrist Institute. https://handandwristinstitute.com/de-quervains-stenosing-tenosynovitis-mommy-thumb-dallas/
- Mustafa, M., Khan, M., Hanif, M., et al. Efficacy of Therapeutic Ultrasound in De-Quervain’ s Tenosynovitis. Pakistan BioMedical Journal. 2022; 5(4). https://doi.org/10.54393/pbmj.v5i4.377
- Bosman, R., Duraku, L.S., van der Oest, M.J.W., et al. Surgical Treatment Outcome of de Quervain’s Disease: A Systematic Review and Meta-analysis. Plastic and Reconstructive Surgery – Global Open. 2022; 10(5): e4305. https://doi.org/10.1097/GOX.0000000000004305
- De Quervain’s Tendinosis. (2023, June 14). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/10915-de-quervains-tendinosis
- Tal, H., Panno, J.M., Vaidyanathan, T.K. Scanning Electron Microscope Evaluation of Wear of Dental Curettes During Standardized Root Planing. Journal of Periodontology.1985; 56(9): 532-536. https://www.ncbi.nlm.nih.gov/pubmed/3897505