Dementia is now known by the term ‘neurocognitive disorder’ or NCD. A patient with a neurocognitive disorder has problems with cognitive functions such as impaired memory, inability to learn or retain information, a distortion of perception, and a loss of problem-solving skills.
Unfortunately, the victims of cognitive decline forget the simplest things that we take for granted. This loss causes so many detrimental health problems, and, unfortunately, dental hygiene is top among the list.
The Problem
Anyone with cognitive impairment has a problem maintaining their oral healthcare. It’s a known fact and a serious problem that health representatives and dental hygienists can verify. Routine hygiene appointments and exams become less and less important as other health issues take center stage.
When parents, siblings, aunts, and uncles can no longer care for themselves, the village must band together to care for and provide support for their everyday needs. These beloved family members may need help going to the bathroom, cooking meals, or brushing their teeth, for example.
It’s either us, the dental professionals, or the various caregivers that work with their loved ones that are tasked with most of these responsibilities, and it can be both intricate and overwhelming in its capacity. Actions we take for granted, like brushing our teeth, can be easily looked over and detrimental to the patient.
Are Oral Health Education For Carers Effective In The Oral Hygiene Management Of Elderly With Dementia? A Systematic Review by Nithin Manchery, Gireesh Kumar Subbiah, et al. studies the effects dental hygiene education has on the health community as they care for patients with dementia, specifically. The researchers believe that incorporating dental hygiene practices in healthcare training will benefit the healthcare professionals, the families, and most importantly, the patients who depend on them.
The Details
While it is true that more recent advances in the health industry are causing people to live and remain active longer than before, this doesn’t take into account that at the end of their lives, they are suffering from a historically high level of cognitive decline. This is because the diseases that would usually lead to death are now being healed, and people are living longer than their brains can function.
Basically, the number of people living with dementia symptoms will triple by the year 2050. As the aging population grows, they retain more of their teeth, which contributes to an increase in the number of oral diseases diagnosed by our dental professionals.
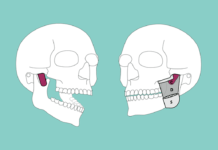
It has been established as a fact that older patients who suffer cognitive decline suffer an increase in dental caries, periodontal disease, infection-related pain, and other health issues. Often a person with dementia does not have the words to express the pain that they feel. With these oral conditions, the pain will develop and will not go away.
In fact, the pain will continue to increase, and the infection may spread throughout the body, causing more problems than we can count. Sometimes deadly problems. An elder with dementia, their family, and their personal healthcare professionals depend on us in the dental community to solve these problems.
The healthcare community concentrates so hard to cure debilitating and deadly diseases in people who end up dying from an infected tooth or a lack of nutrition due to the inability to eat. This defeats the purpose, and so the researchers of this article have deemed it necessary to call for an inclusion of basic dental hygiene care in all forms of healthcare education.
For this study, nursing students were broken up into groups, one that was given oral hygiene education and one that was not. These groups were followed for a short while, and their patients were given oral check-ups to mark changes and progress. The results were exactly what one would expect from such a study. Those with the education completed the tasks they were educated on, and those who were not, were lost and did not, on the whole, complete any of the oral hygiene goals on their patients.
The Solution
Healthcare workers said that they had a lack of motivation to care for their patient’s teeth. Some also cited an ‘ick-factor’ that prevented them from maintaining their patient’s oral health care. Nurses who were given education on oral health and the necessary hygiene maintenance procedures were much more motivated and confident to care for their patients’ oral needs and cited that evidence-based strategies within the education they received were the greatest motivating factors.
The patients of these nurses, compared to those of the nurses who did not get the oral hygiene training, were much better off when it came to the less serious dental concerns, such as gingivitis, plaque, denture hygiene, tongue coating, and tongue discoloration. It was too soon to document effects on caries and periodontal disease, but logic dictates that an increased hygiene level in general, as shown by the patients, will affect those rates when further evaluated.
For the record, these classes should be added to and changed to include and reflect ways to deal with the psychological problems associated with dementia patients and their resistance to receiving help with their oral hygiene. But that’s another story.