Disclosure: This article is sponsored content from Designs for Vision as part of our sponsored partner program.
The prevalence of musculoskeletal disorders (MSDs) in the dental profession is well established and can have detrimental effects on productivity and lead to early retirement. The cause is attributed to ergonomic hazards, such as strained posture and repetitive movements. Studies show MSDs occur in 54-93% of dental professionals and involve the spine, shoulders, and hand-wrist tract.1 Though that statistic is a wide range, it is astounding nonetheless.
Dental professionals are aware of the pain they feel. Unfortunately, many people, including family members and patients, don’t seem to understand the strain this profession puts on the human body. I had a professor in hygiene school tell me if a patient says they can’t lie back, you need to tell them, “Sir/Ma’am, I have to do this for eight hours today, you only have to lie back for about an hour.” Of course, I have never said this to a patient, but every time I have a patient that can’t lie back, and I’m forced to become a contortionist to care for them properly, I hear her words in my head.
The list of occupational hazards for dental professionals is not limited to musculoskeletal disorders; it also includes stress and burnout, vision-related health issues, percutaneous injury, noise, mercury-related health problems, allergies, and infection to name just a few. A review of these occupational health-related problems concluded the most frequently reported was musculoskeletal disorders.2
A contributing factor in the musculoskeletal disorders in dental professionals is prolonged static posture. Prolonged static postures are inherent in dentistry. Awkward postures that involve forward bending and repeated rotation of the head, neck, and trunk to one side, are common occurrences during clinical work. As posture deviates more from neutral, the muscles which are responsible for the preferred side of rotating or bending become stronger, and the matching antagonistic muscles become elongated and weakened, creating a muscle imbalance.
Muscles that are under stress from prolonged static posture are also susceptible to ischemia, due to the prolonged contraction and following fatigue. Under normal conditions, damaged tissues are repaired during periods of rest. However, in dentistry the rate of damage exceeds the rate of repair due to insufficient rest periods, potentially leading to necrosis of the muscle. In an effort to protect the stressed area from further pain or injury, the body compensates by using another part of the muscle to maintain posture. This is known as muscle substitution. Muscle substitution is a self-perpetuating cycle; tighter muscles become tighter, and weaker muscles become weaker. This can result in the development of a whole range of musculoskeletal disorders.3
Below are some suggested precautions to employ to prevent and or reduce musculoskeletal disorders.

Operator and patient positioning: Although some surveys indicate regardless of the operator position used, the majority of practicing dental hygienists developed musculoskeletal disorders.4 Other research suggests alternating between standing and sitting. Standing uses different muscle groups than sitting, therefore, alternating between the two positions will allow one group of muscles to rest while the workload is shifted to another group of muscles.
Repositioning the feet can be helpful too. Subtle changes in foot position can shift the workload from one group of lower back muscles to another, allowing the overworked tissues to be replenished with nutrients. Positioning patients at the proper height is another precaution to employ. Operators should take the time to position their patients properly for maxillary or mandibular procedures. Also, consider using a saddle-style operator stool that promotes the natural lower back curve by increasing the hip angle.5
Instruments: Instrument diameters range from 5.6 to 11.5mm, larger handle diameters reduce hand muscle load and pinch force. A round handle compared to a hexagonal handle will reduce muscle force and compression. Lightweight instruments also reduce muscle workload and pinch force. Balance is important to reduce hand muscle fatigue; fulcruming on a third digit rest compared to a fourth digit rest does not engage the wrist as much while guiding and positioning the instrument or handpiece. Knurled handles such as diamond shaped, or crisscross patterns serve to reduce pinch grip due to increased tactile sensation. Sharp instruments are essential for effective and efficient patient care.6
Glove size: Although the influence of gloves on hand discomfort has yet to be explored, it has been directly cited as a potential contributing factor in carpal tunnel syndrome. Ambidextrous or non-hand specific gloves exert more force than fitted gloves across the palmar region of the hand and may exacerbate symptoms of carpal tunnel syndrome. Therefore, hand-specific gloves are recommended; they fit better and places less force on hands.6
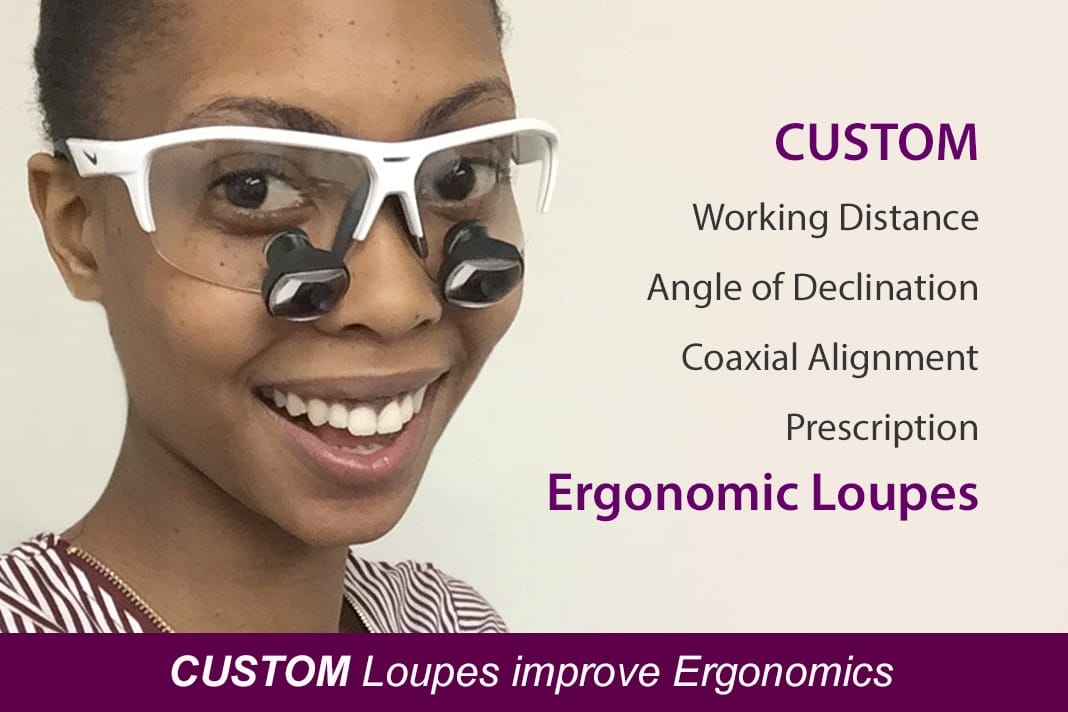
Well fitting Loupes: Proper selection, adjustment, and use of magnification systems have been associated with decreased neck and low back pain, as they allow operators to maintain healthier postures.5
Appropriate patient scheduling: Scheduling patients should be done in a manner that allows the hygienist periodic breaks. During these breaks, hygienists should practice doing chairside directional stretching. Stretches performed in the opposite direction of the awkward prolonged static posture may prevent muscle imbalances which can lead to pain and MSDs. Directional stretches can be performed in or out of the operatory and can be incorporated into a daily routine that facilitates balanced musculoskeletal health. Directional stretching involves a rotation, side bending or extension component that generally is in the opposite direction of that in which the operator frequently works.
Frequent stretching breaks address the detrimental physiological changes that can develop while working in less than optimal or awkward prolonged static postures: ischemia, trigger points, muscle imbalances, joint hypomobility, nerve compression, and disk degeneration. Furthermore, stretching increases blood flow to muscles, increases production of joint synovial fluid, reduces the formation of trigger points, maintains normal joint range of motion, increases nutrient supply to vertebral disks, creates a relaxation response in the central nervous system, and warms up the muscle before beginning to work.5
Exercise: Musculoskeletal disorders in dentistry often begin with fatigue of the postural stabilizing muscles of the trunk and shoulders. As these muscles fatigue, operators tend to slump into poor posture, setting the stage for injuries. Hygienists should perform specific strengthening exercises for the trunk and shoulder girdle to enhance the health and integrity of the spinal column, maintain good overworking posture, optimize the function of the arms and hands to help prevent injuries.
Aerobic exercise should be performed three to four times a week for at least 20 minutes. One major contributing factor to musculoskeletal disorders is a decreased flow of nutrients and oxygen to muscles. Aerobic exercise increases blood flow to all the tissues in the body and improves their ability to use oxygen. In addition, aerobic exercise improves cardiovascular and cardiorespiratory function, lowers heart rate and blood pressure, increases high-density lipoprotein (good) cholesterol, decreases blood triglycerides, reduces body fat, improves stress tolerance, increases mental acuity, improves sleep quality, and may increase longevity. Operators should choose aerobic exercises that they enjoy.5
Stress management: Stress can elicit muscular contraction and pain, especially in the trapezius muscle. Operators may use various stress-reduction techniques to decrease stress-related muscular tension. They include breathing techniques, progressive relaxation, visualization, massage, aerobic exercise, meditation or yoga.5
Proper temperature: It is recommended that hands and fingers be kept above 25°C or 77°F to avoid detrimental effects on dexterity and grip strength.6
According to the Bureau of Labor Statistics, in 2013 musculoskeletal disorder cases accounted for 33% of all worker injury and illness cases. The Bureau of Labor Statistics defines musculoskeletal disorders to include cases where the nature of the injury or illness is:
- Pinched nerve
- Herniated disc
- Meniscus tear: sprains, strains, tears,
- Hernia (traumatic and nontraumatic): pain, swelling, and numbness
- Carpal or tarsal tunnel syndrome
- Raynaud’s syndrome or phenomenon
- Musculoskeletal system and connective tissue diseases and disorders
- When the event or exposure leading to the injury or illness is overexertion and bodily reaction, (unspecified), overexertion involving outside sources, repetitive motion involving microtasks, other and multiple exertions or bodily reactions
- Rubbed, abraded, or jarred by vibration.7
I personally feel musculoskeletal disorder cases are underreported in the dental field. To add insult to injury, many dental hygienists deal with musculoskeletal disorders which require treatment, however, medical insurance is not a standard benefit in dentistry. This causes financial strain on many dental hygienists. Taking as many precautions as possible to reduce the risk and further damage of musculoskeletal disorders is a must in this profession.
Many studies state musculoskeletal disorders can start during hygiene/dental school.8 More emphasis on prevention and proper care should be added to the curriculum, as well as follow up continuing education, on this topic. As more research is done, there will hopefully be more options to reduce musculoskeletal disorders in the dental profession. The profession has come a long way, but it is imperative to stay informed and practice proper ergonomics to improve health and reduce injury and early retirement.
LIMITED TIME ONLY: Experience Better Posture and Ergonomics with a 45-Day Free Trial of Loupes!
Resources
- Simone De Sio, Veronica Traversini, Francesca Rinaldo, Valerio Colasanti, Giuseppe Buomprisco, Roberto Perri, Federica Mormone, Giuseppe La Torre, and Fabrizio Guerra. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: an umbrella review. PeerJ. 2018; 6. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5772380/
- Rajeshree Moodley, Saloshni Naidoo, and Jacqueline van Wyk. The prevalence of occupational health-related problems in dentistry: A review of the literature. J Occup Health. 2018 Mar 20; 60(2): 111–125. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5886878/
- Andrew Ng, Melanie J. Hayes, and Anu Polster. Musculoskeletal Disorders and Working Posture among Dental and Oral Health Students. Healthcare (Basel). 2016 Mar; 4(1): 13. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4934547/
- Barry RM, Spolarich AE, Weber M, Krause D, Woodall WD, Bailey JH. Impact of Operator Positioning on Musculoskeletal Disorders and Work Habits among Mississippi Dental Hygienists. J Dent Hyg. 2017 Dec; 91(6):6-14. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29378801
- Amandeep Chopra. Musculoskeletal Disorders in Dentistry – A Review. JSM Dent 2014; 2(3): 1032. Retrieved from https://www.jscimedcentral.com/Dentistry/dentistry-2-1032.pdf
- Praveen S. Jodalli, Suchi Kurana, Shameema, Mallikarjuna Ragher, Jaishree Khed, and Vishnu Prabhu. Posturedontics: How does dentistry fit you? J Pharm Bioallied Sci. 2015 Aug; 7(Suppl 2): S393–S397 Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606627/
- United States Department of Labor/Occupational Safety and Health Administration. Retrieved from https://www.osha.gov/SLTC/ergonomics/index.html
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014 Feb; 88(1):36-41. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/24563051











