Hypertension affects about half of the population worldwide, and poor oral health appears to worsen blood pressure and impedes hypertension treatment.1 High blood pressure (HBP) and sleep apnea coexist with many of our patients suffering.2,3
Following the standard of care, we take blood pressure on every patient, every visit, but what do we do with that information after we record it in their chart is a question. When speaking about the harmful effects of high blood pressure, I personally have been amiss in sharing how to help our patients.
What options should we explore in the office, and is it out of our scope to share ideas on how to lower blood pressure? Never contradicting their current use of any prescribed medications, of course, but we may be able to offer helpful suggestions. First and foremost, it is a must to verbally tell the patient their blood pressure and understand practice protocol regarding when to refer to a physician or suspend treatment if the pressure is too high. Write it down and give it to the patient or let them put it in their phone if they want to share it with their physician.
Trust has a central role in healthcare encounters, and in dentistry, the dentist or hygienist’s relationship is more of an interpersonal relationship vs. institutional. Recognizing the patient’s vulnerability and doing what is best for the patient’s overall health and well-being should be central if or when making recommendations.
Approaches
The DASH diet, a dietary approach to decrease hypertension, is well-studied and extremely useful for patients to lower their blood pressure.4 Not shocking, the diet consists of vegetables, fruits, lean meats, nuts, seeds, and lowering salt. Perhaps have a printout describing the diet or sources to give the patient if the conversation yields that direction.
Hibiscus tea shows great results for not only blood pressure but the antioxidants in hibiscus tea abounds. Research for diabetic patients and hibiscus tea shows a positive result, but, as always, patients should check with their physicians.5,6 Lowering salt sounds simple and helps, but if you have eaten anything out of a box or a can, decreasing salt intake is clearly not that easy.7
What caught my eye recently was a simple therapy that could be another area we may be able to advance our healthcare reach with hypertensive patients.
The number one killer for both men and women is cardiovascular (CV) disease. High blood pressure elevates not only that risk but is a companion to chronic kidney disease and diabetes. High-resistance inspiratory muscle strength training (IMST) is a low-tech, affordable therapeutic that could play a key role in helping aging adults reduce their CV risk.
This therapy was developed in the 1980s to help those who endure respiratory issues. However, IMST is also used by runners, cyclists, and swimmers. People with Parkinson’s, amyotrophic lateral sclerosis (ALS), multiple sclerosis, and chronic obstructive pulmonary disease (COPD) can see benefits when used as an adjunctive therapy to improve ventilation and respiratory strength.8
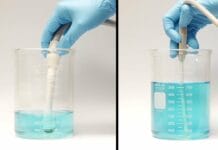
Using a handheld device, you inhale hard, and the device provides resistance; all the while, it strengthens your breathing muscles and your diaphragm. The author of a significant paper, Dr. Daniel Craighead, that described the benefits of IMST mentioned that the co-founder of Headspace, Andy Puddicombe, does his breathing while on the app for five minutes daily. Quite an easy and simple addition.
Craighead’s research found participants drop nine points on average for systolic pressure with a modest drop in diastolic after six weeks of therapy. Participants also had a 45% improvement in endothelial function with improved nitric oxide (NO) bioavailability levels. NO is a signaling molecule for CV function. Furthermore, they saw lowered inflammation (c-reactive protein) and oxidative stress but, unfortunately, no improvement in arterial stiffness.9 Another study also found that IMST lowers blood pressure and systemic vascular resistance – the amount of force exerted on circulating blood by the vasculature of the body.10
Sleep Apnea
Sleep-disordered breathing has horrible health outcomes from immune dysfunction, cognition problems, hypertension, and CVD.11 Obstructive sleep apnea (OSA) can activate the central nervous system and increase catecholamines production.
Catecholamines are released in response to physical or emotional stress; they enter the bloodstream to trigger your body’s fight or flight response. Catecholamines include epinephrine (adrenaline), norepinephrine, and dopamine. After using the hormones, your body eliminates the remaining waste through urine. The elevation is greater in patients with severe sleep apnea and hypertension.
Recent findings in the Journal of Clinical Hypertension found that continuous positive airway pressure (CPAP) in patients with sleep apnea reduces “catecholamines levels and blood pressure suggesting sympathetic activity plays an intermediary role in the relationship between OSA‐related stress and hypertension.”12 Results from 2016 research showed that IMST could modify blood pressure and plasma catecholamines in people with ongoing nighttime apnea and hypoxemia.13 If we are in a sleep solution dental practice, another place to explore is IMST.
In Closing
Blood pressure is a public health crisis, and we can make even more of an impact on our patients. If you happen to work in a sleep-focused dental practice, IMST may be another good alternative, or as I just did, order one for myself and my husband. It only takes five minutes (five sets of six breaths-in, with one minute of rest between sets), six days a week for six weeks, to see marked results.
If you or a loved one has type 2 diabetes, the University of Arizona is beginning a clinical trial to investigate IMST therapy and adults with recent-onset type 2 diabetes.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Desvarieux, M., Demmer, R.T., Jacobs, D.R. Jr, et al. Periodontal Bacteria and Hypertension: The Oral Infections and Vascular Disease Epidemiology Study (INVEST). J Hypertens. 2010; 28(7): 1413-1421. https://pubmed.ncbi.nlm.nih.gov/20453665/
- Wang, Y., Shou, X., Wu, Y., et al. Relationships Between Obstructive Sleep Apnea and Cardiovascular Disease: A Bibliometric Analysis (2010-2021). Med Sci Monit. 2022; 28: e933448. https://pubmed.ncbi.nlm.nih.gov/34975145/
- Konecny, T., Kara, T., Somers, V.K. Obstructive Sleep Apnea and Hypertension: An Update. Hypertension. 2014; 63(2): 203-209. https://pubmed.ncbi.nlm.nih.gov/24379177/
- Chiavaroli, L., Viguiliouk, E., Nishi, S.K., et al. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients. 2019; 11(2): 338. https://pubmed.ncbi.nlm.nih.gov/30764511/
- Serban, C., Sahebkar, A., Ursoniu, S., et al. Effect of Sour Tea (Hibiscus sabdariffa L.) on Arterial Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Rrials. J Hypertens. 2015; 33(6): 1119-1127. https://pubmed.ncbi.nlm.nih.gov/25875025/
- Mozaffari-Khosravi, H., Jalali-Khanabadi, B.A., Afkhami-Ardekani, M., et al. The Effects of Sour Tea (Hibiscus sabdariffa) on Hypertension in Patients with Type II Diabetes. J Hum Hypertens. 2009; 23(1): 48-54. https://pubmed.ncbi.nlm.nih.gov/18685605/
- Filippini, T., Malavolti, M., Whelton, P.K., et al. Blood Pressure Effects of Sodium Reduction: Dose-Response Meta-Analysis of Experimental Studies. Circulation. 2021; 143(16): 1542-1567. https://pubmed.ncbi.nlm.nih.gov/33586450/
- Ferreira, G.D., Costa, A.C., Plentz, R.D., et al. Respiratory Training Improved Ventilatory Function and Respiratory Muscle Strength in Patients with Multiple Sclerosis and Lateral Amyotrophic Sclerosis: Systematic Review and Meta-Analysis. Physiotherapy. 2016; 102(3): 221-228. https://pubmed.ncbi.nlm.nih.gov/27026167/
- Craighead, D.H., Heinbockel, T.C., Freeberg, K.A., et al. Time-Efficient Inspiratory Muscle Strength Training Lowers Blood Pressure and Improves Endothelial Function, NO Bioavailability, and Oxidative Stress in Midlife/Older Adults with Above-Normal Blood Pressure. J Am Heart Assoc. 2021; 10(13): e020980. https://pubmed.ncbi.nlm.nih.gov/34184544/
- DeLucia, C.M., De Asis, R.M., Bailey, E.F. Daily Inspiratory Muscle Training Lowers Blood Pressure and Vascular Resistance in Healthy Men and Women. Exp Physiol. 2018; 103(2): 201-211. https://pubmed.ncbi.nlm.nih.gov/29178489/
- Punjabi, N.M., Caffo, B.S., Goodwin, J.L., et al. Sleep-disordered Breathing and Mortality: A Prospective Cohort Study. PLoS Med. 2009; 6(8): e1000132. https://pubmed.ncbi.nlm.nih.gov/19688045/
- Green, M., Ken-Dror, G., Fluck, D., et al. Meta-analysis of Changes in the Levels of Catecholamines and Blood Pressure with Continuous Positive Airway Pressure Therapy in Obstructive Sleep Apnea. J Clin Hypertens. 2021; 23(1): 12-20. https://pubmed.ncbi.nlm.nih.gov/32970922/
- Vranish, J.R., Bailey, E.F. Inspiratory Muscle Training Improves Sleep and Mitigates Cardiovascular Dysfunction in Obstructive Sleep Apnea. Sleep. 2016; 39(6): 1179-1185. https://pubmed.ncbi.nlm.nih.gov/27091540/