As a dental hygienist, I thought I had a decent overall understanding of the human body since our curriculum includes biology, chemistry, anatomy, and physiology. One day out of the blue, I experienced abdominal pain so severe I thought it was a severe acid reflux attack.
It was a little strange for me because, if I occasionally get a mild stomachache, I can take an antacid and feel relief in minutes. This was different. The pain was so severe that the antacids didn’t help. For hours, I couldn’t lay down or find a comfortable position to sit. It hurt to breathe, I was very bloated, and the pain went into my upper back.
I made an appointment right away, and my doctor prescribed a daily antacid which helped for about two months until the same pain flared up again.
This time I went to the emergency room. Describing my symptoms to the nurses and doctors, I wondered, is this what a stomach ulcer feels like? I vaguely remembered learning about Helicobacter pylori in microbiology. Nonetheless, I just wanted an answer after the CAT scan and ultrasound because if this pain flared up again, I wouldn’t be able to cope.
I was shocked to learn I had gallstones in my gallbladder. I was almost embarrassed to not really know what the gallbladder does, what causes gallstones, or that one could even live without a gallbladder.
Formation of Gallstones
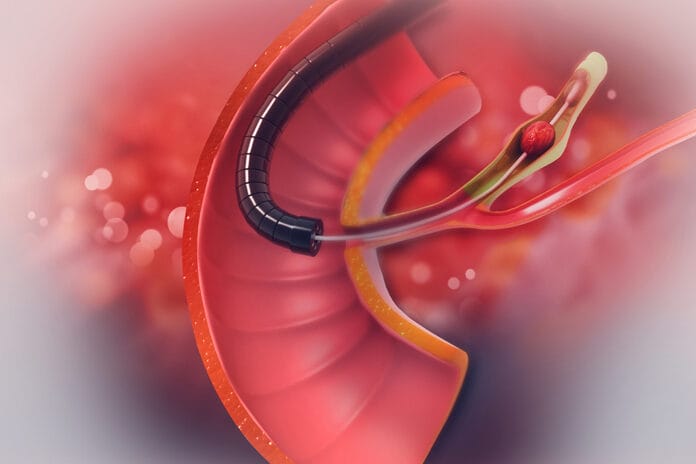
The gallbladder is attached to the liver and stores bile. Bile emulsifies fats in our diets. “Bile mainly consists of water (90%) and three lipid species: cholesterol (4% of solutes by weight), phospholipids (24%) and bile salts (72%).”1 Gallstones are calcified bile that blocks the ducts. “The majority (80% to 90%) of gallstones formed within the gallbladder consist mainly of cholesterol (70%) in a matrix of bile pigments, calcium salts, and glycoproteins.”2 The medical terminology for gallstones is cholelithiasis.
Oral-Systemic Connection
Dental hygienists understand that a high-fat diet can harm the liver, and there is an oral-systemic correlation between periodontitis and liver health.
“Increasing evidence indicates that periodontitis may participate in the progression of liver diseases, such as non-alcoholic fatty liver disease, cirrhosis, and hepatocellular carcinoma, as well as affecting liver transplantation.”5
When talking to dental patients about a healthy diet to control caries, etc., we can also mention a diet high in sugar and fat puts strain on bile production, which can contribute to gallstones. A hospital-based control study performed by Mahsa Jessri and Bahram Rashidkhan specified an unhealthy diet as a high intake of refined grain, tea, sugar, red meat, solid fat, soft drinks, baked potatoes, snacks, processed meats, high-fat dairy products, eggs, salt, pickled foods and sauerkraut, and low intake of coffee.7 Gallstones have for many years been considered a significant public health problem and are expensive to treat.8
Moreover, recent research within the past couple of years has tried to establish a direct connection between oral hygiene and gallstones. An article published in June 2020 establishes “the microbiome of bile correlates with the bacterial composition of saliva, and the microbiome of the biliary tract has a high similarity with the microbiota of the duodenum. Pathogenic microflora of the oral cavity, through mechanisms of immunomodulation, can affect the motility of the gallbladder and the expression of mucin genes and represent one of the promoters of stone formation in the gallbladder.”8 This is a very important finding for dental health professionals to be aware of. In layman’s terms, the study found that the bacteria common to the oral cavity are limiting the ability of the gallbladder to contract and produce mucus gels through immunosuppression, which contributes to gallstones.
In addition, an article published in 2017 in the European Journal of Gastroenterology and Hepatology studied an association between oral hygiene and gallstones in the U.S. population. In this study, adults with gallstone disease differed from those without gallstones in terms of age, sex, and oral hygiene.9 “There was significant association of gallstone disease with poor to fair oral hygiene.”9
Gender Influence
The group with the highest risk for gallstones, however, is one you might not expect. “In all populations of the world, regardless of overall gallstone prevalence, women are almost twice as likely as men to experience cholelithiasis. Gender is one of the most powerful influences on gallstones, which are more common in females during their fertile years as in males.”6
Women of childbearing age who have had a pregnancy are most at risk, and there is a correlation to the number and age of pregnancies.6 Another study found that hormone-led birth control can also be a factor.3 There are subpopulations of women susceptible to the early formation of gallstones after exposure to either oral contraceptives or pregnancy.3
As if the hormones couldn’t wreak enough havoc on women, estrogen can also contribute to gallstones. This is due to “how the liver metabolizes cholesterol in response to estrogen. A large number of human and animal studies have proposed that estrogen increases the risk of developing cholesterol gallstones by increasing the hepatic secretion of biliary cholesterol, which, in turn, leads to an increase in cholesterol saturation of bile.”10 This is why estrogen treatments can also contribute to gallstones. “An increased hepatic secretion of cholesterol results in increased cholesterol saturation of bile and an enhanced rate of gallstone formation during estrogen treatment.”4
While we are talking to our pregnant patients about xerostomia, increased risk of caries, and the hormones inflaming the gingiva, we can also mention how a feeling of more severe acid reflux, bloating, and upper back pain could be gallstones from those same hormones. Symptoms of gallstones can vary and even be asymptomatic, but abdominal with upper back pain is common.
My personal experience with gallstones was due to pregnancy hormones. The doctors found gallstones so large that they recommended a cholecystectomy, total removal of the gallbladder.
I quickly agreed to the surgery to be out of pain but then wondered how my life would change in the future. My doctor assured me that patients could live full, healthy lives without a gallbladder. However, I should probably avoid high fat and greasy foods as the digestive tract has a difficult time digesting fats without bile. In an interesting coincidence, one of my nursing aides also had her gallbladder removed after her pregnancy.
Need CE? Click Here to Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Carey, M.C., Lamont, J.T. Cholesterol Gallstone Formation. 1. Physical-chemistry of Bile and Biliary Lipid Secretion. Prog Liver Dis. 1992; 10: 139-63. PMID: 1296228. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1296228/
- Paumgartner, G., Sauerbruch, T. Gallstones: Pathogenesis. The Lancet. 1991; 338(8775): 1117–21. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/014067369191972W
- Scragg, R.K., McMichael, A.J., Seamark, R.F Oral Contraceptives, Pregnancy, and Endogenous Oestrogen in Gall Stone Disease–A Case-control Study. Br Med J (Clin Res Ed). 1984; 288: 1795–9. Retrieved from https://www.bmj.com/content/288/6433/1795.abstract
- Henriksson, P., Einarsson, K., Eriksson, A., et al. Estrogen-induced Gallstone Formation in Males. Relation to Changes in Serum and Biliary Lipids during Hormonal Treatment of Prostatic Carcinoma. The Journal of Clinical Investigation. Retrieved from https://www.jci.org/articles/view/114240
- Han, P., Sun, D., Yang, J. Interaction between Periodontitis and Liver Diseases. Biomedical Reports. 2016; 5(3): 267-276. doi:10.3892/br.2016.718. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998044/
- Acalovschi, M. Cholesterol Gallstones: From Epidemiology to Prevention. Postgraduate Medical Journal. 2001; 77: 221-229. Retrieved from https://pmj.bmj.com/content/77/906/221
- Jessri, M., Rashidkhani, B. Dietary Patterns and Risk of Gallbladder Disease: A Hospital-based Case-control Study in Adult Women. Journal of Health, Population, and Nutrition. 2015; 33(1): 39-49. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4438647/
- Grigor’eva, I.N., Romanova, T.I. Gallstone Disease and Microbiome. 2020 Jun 2; 8(6): 835. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32498344/
- Bhandari, S., Reddy, M., Shahzad, G. Association between Oral Hygiene and Ultrasound-confirmed Gallstone Disease in U.S. Population. European Journal of Gastroenterology and Hepatology. 2017; 29(7): 861-862. Retrieved from https://journals.lww.com/eurojgh/Citation/2017/07000/Association_between_oral_hygiene_and.19.aspx
- Wang, H.H., Liu, M., Clegg, D.J., Want, D.G. New Insights into the Molecular Mechanisms Underlying Effects of Estrogen on Cholesterol Gallstone Formation. Biochimica et Biophysica Acta. 2009; 1791(11): 1037-47. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2756670/