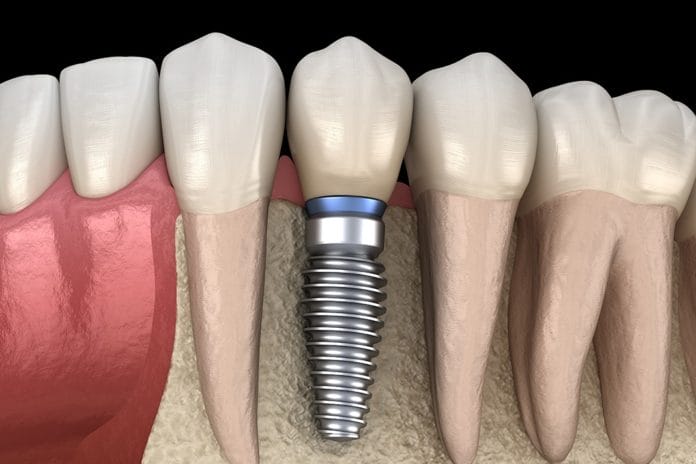
According to the American Academy of Implant Dentistry, 500,000 dental implants are placed in the United States annually.1 As dental hygienists, the number of patients we treat who have at least one dental implant will increase. For this reason, it is important for dental hygienists to become familiar with dental implants from both restorative and preventive aspects.
We need to be able to educate ourselves and our patients on some of the complications encountered with implants. These issues will arise in all of our dental practices.
Abutment Screw Loosening
According to one study, abutment screw loosening is the “most common mechanical complication associated with implant-supported restorations.”2 A patient may present with concern that their implant is loose and will need to be removed. But this is rarely the case.
If the abutment and crown around an implant are loose, it is easily detected, similar to the way you would check for mobility on a normal tooth. I typically use the blunt end of my hand mirror and my probe and gently apply pressure both buccal and lingual.
Depending on what type of practice you work in, your dentist may be able to fix this for the patient in the office. However, the patient may also need to be referred back to the doctor who placed the restoration if it wasn’t your doctor, or possibly a specialist such as a prosthodontist.
Excessive Occlusal Trauma
Excessive occlusal trauma is another complication that can arise with dental implants. This can happen when a patient clenches and/or grinds because the implant cannot tolerate the excessive forces generated during these movements.3
The main reason this excessive trauma can cause complications with an implant is because there is a lack of a periodontal ligament with an implant. The occlusal forces are applied directly to the surrounding bone of the implant, which puts them at a greater risk for a fracture and/or screw loosening.
Checking the occlusion of implants should be done just as we check the occlusion of natural teeth.
Poor Biofilm Control and Lack of Regular Maintenance Therapy
Oral hygiene can be a huge factor in the success or failure of a dental implant − something we can become experts at discussing with our patients. One study compared two different electric toothbrushes, a manual toothbrush, and an air-flosser to determine the best adjunct to help keep implants clean. The study concluded that all of the tools were similarly effective except for the manual toothbrush. The study went on to say that oral hygiene is important for the long-term stability of implants.4
We cater our dental hygiene recommendations to our patients based on their needs. If they have one or multiple dental implants, this is something we should consider as well.
When individualizing home-care instruction for implants, it may be prudent to toss the floss. Research states, “The remnants of floss in the peri-implant sulcus have also been regarded as a triggering factor for peri-implantitis. Van Velzen et al. reported 10 cases with progressive peri-implantitis related to floss remnants. Interestingly, in 90% of the cases, the inflammation resolved spontaneously after mechanical removal of the floss remnants. Thus, caution is required when providing personal oral hygiene instructions involving the use of floss, and patients should be further encouraged to employ interproximal brushes.”6
Keep in mind when suggesting the use of interdental brushes that they need to be individually sized for the patient’s embrasure space(s). To avoid implant surface alterations and scratches, make sure the recommended interdental brush is plastic or that any metal is coated to avoid scratching the implant surface. Scratches increase surface area in which bacteria can thrive.
The American Academy of Periodontology compared numerous studies comparing the link between oral hygiene as well as preventative maintenance care for implants, and determined that “There is evidence that poor plaque control and lack of regular maintenance therapy constitute risk factors/indicators for peri-implantitis.”
Peri-implantitis is defined as changes in the level of the crestal bone in conjunction with bleeding on probing and can be accompanied by deeper probe depths. Suppuration may be present as well.5 Titanium scalers are best for cleaning around implants because they do not leave behind residue on the surface as plastic implant scalers may, which can lead to peri-implantitis.
Set a Protocol
Setting a protocol for your patients with dental implants is a good idea. If a complication like peri-implantitis arises, you can treat it earlier. Some offices make it part of their routine care for their implant patients to take a yearly PA of implants to ensure the bone level is staying the same. You may want to evaluate occlusion, check for mobility, and probe depths in a similar way.
We can all appreciate the time crunch hygienists face, so making your protocol something quick and easy but thorough should be an important parameter for how you determine what you’re going to do for your patients.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Sadowsky, S.J. Occlusal Overload with Dental Implants: A Review. International Journal of Dental Implant Dentistry. 2019; 5(29). https://journalimplantdent.springeropen.com/articles/10.1186/s40729-019-0180-8
- Lee, J., Cha, H. Screw Loosening and Changes in Removal Torque Relative to Abutment Screw Length in a Dental Implant with External Abutment Connection after Oblique Cyclic Loading. Journal of Advanced Prosthodontics. 2019; 10(6): 415-421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6302080/
- Gupta, S., Gupta, H., Tandan, A. Technical Complications of Implant-causes and Management: A Comprehensive Review. National Journal of Maxillofacial Surgery. 2015; 6(1): 3-8. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4668729/
- Maeda, T., Mukaibo, T., Masaki, C., Thongpoung, S., et al. Efficacy of Electric-powered Cleaning Instruments in Edentulous Patients with Implant-supported Full-arch Fixed Prostheses: A Crossover Design. International Journal of Implant Dentistry. 2019; 5(7). https://journalimplantdent.springeropen.com/articles/10.1186/s40729-019-0164-8
- Soldatos, N., Romanos, G.E., Michaiel, M. et al. Management of Retrograde Peri-Implantitis Using an Air-Abrasive Device, Er, Cr:YSGG Laser, and Guided Bone Regeneration. Case Reports in Dentistry. 2018; 2018(7283240). https://www.hindawi.com/journals/crid/2018/7283240/cta/
- Monje, A., Insua, A. Wang, H. Understanding Peri-Implantitis as a Plaque-Associated and Site-Specific Entity: On the Local Predisposing Factors. J Clin Med. 2019; 8(2): 279. https://www.researchgate.net/publication/306119789_Comparison_Between_Interdental_Brush_and_Dental_Floss_for_Controlling_Interproximal_Biofilm_in_Teeth_and_Implants