Lupus erythematosus (LE) is a complex autoimmune disease that can affect multiple organ systems, including the oral cavity. Although the etiology remains unknown, it seems to be influenced by genetic and environmental factors. Oral signs often present early, and patients may also experience systemic symptoms such as fatigue, fever, and weight loss. These signs and symptoms may first be noticed during routine dental visits. For many patients, oral lesions are among the earliest signs, while xerostomia and mucosal pain are frequent and persistent manifestations of the disease. Dental hygienists are uniquely positioned to identify these manifestations, making their role in early detection and ongoing management essential.1
A chronic connective tissue disease, LE can be classified into two major types that can occur together or separately: systemic lupus erythematosus (SLE) and cutaneous lupus erythematosus (CLE). CLE can be further divided into three subtypes: acute cutaneous lupus erythematosus (ACLE), subacute cutaneous lupus erythematosus (SCLE), and chronic cutaneous lupus erythematosus (CCLE).2
SLE involves multiple organs, while CCLE often presents as localized skin and mucosal disease, including oral discoid lesions.1,3 Classification criteria by the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) emphasize that mucocutaneous manifestations are a core domain of SLE.4 The underlying disease pathology directly contributes to the oral findings observed in dental settings.1
ACR guidelines highlight that disease activity and associated treatments, such as corticosteroids, antimalarials, and biologic agents, directly impact oral findings and dental care considerations.5,6 Understanding a patient’s specific diagnosis – SLE, CCLE, or overlapping conditions like secondary Sjögren’s syndrome – helps dental professionals anticipate complications such as xerostomia and increased caries risk.1,7,8
Microbial dysbiosis, particularly in subgingival biofilm, may also contribute to systemic inflammation and autoimmune activation in lupus, emphasizing the importance of periodontal health in this population.9 Understanding the impact of lupus on oral health enables dental hygienists to provide more informed and compassionate care.
Common Oral Manifestations of Lupus
Oral manifestations are often among the first signs of lupus. Common clinical findings include xerostomia, mucosal pain, and oral lesions, which may appear before, during, or after the systemic diagnosis.1,7 Dental hygienists may notice these early oral indicators during routine oral tissue screenings.
Among these oral manifestations, xerostomia is a frequent and persistent problem, often resulting from the common comorbidity, secondary Sjögren’s syndrome.7 Hyposalivation significantly contributes to patient discomfort and increased caries risk.1,8
The overall prevalence of oral mucosal lesions is estimated at 31%. Of that, oral ulcers are the most frequently reported, affecting approximately 30% of patients.10 Ulcers typically present as single or multiple aphthous-like superficial lesions that appear pale yellow to grayish-white with a peripheral red rim (see Image 1). Frequently located on the palate, buccal mucosa, or tongue, they often cause pain when irritated.1,3,10

Other common findings include erythema, glossodynia, and cheilitis.1,3,10 Lupus cheilitis is an inflammatory condition usually affecting the vermilion border of the lower lip. It typically presents as a small or diffuse erythematous and edematous lesion that may progress into painful, crusty ulcers.3
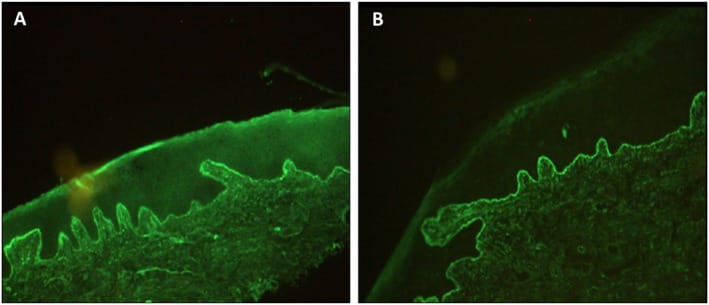
Patients may also present with discoid lesions, which can appear on the buccal mucosa and lips. These lesions feature white striae (“brush border” pattern), which have a clinical appearance that resembles oral lichen planus (see Image 2).1,3

Courtesy of Rodsaward, P., et al.12 Cropped from the original. (CC BY-NC 4.0)
Clinically, distinguishing between discoid lesions and oral lichen planus is difficult due to their similar presentation of reticular white striations, atrophic zones, and erosive surfaces.3 A definitive diagnosis requires a biopsy with histopathologic and immunofluorescent evaluations due to their distinct inflammatory patterns.3,13 Lupus lesions typically exhibit band-like interface dermatitis with basal cell degeneration and the deposition of immunoreactants (immunoglobulins or complement proteins) along the basement membrane, a feature known as the lupus band (see Image 3).13
Given the diagnostic challenge and the significant differences in treatment and systemic implications, dental hygienists should refer patients with ambiguous or recurrent lesions, especially when accompanied by systemic symptoms, for biopsy and rheumatologic or dermatologic evaluation.3,4
These oral complications can significantly impair nutrition, speech, and quality of life.1 The ability to differentiate lupus manifestations from other oral pathologies is essential to adapt care plans to patients’ systemic status and medications.1,3
Oral Complications from Lupus and Medications
Beyond direct mucosal involvement, lupus and its treatments can contribute to a variety of oral complications. Immunosuppressive agents, such as corticosteroids, methotrexate, or biologic agents, can impair wound healing and increase susceptibility to infection.6 Secondary infections, including candidiasis and periodontitis, are common and often arise from immunosuppression induced by systemic drug therapies.1,8
Patients with lupus have been found to exhibit elevated antibody titers against pathogenic periodontal bacteria such as A. actinomycetemcomitans and P. gingivalis. These titers correlate with anti-dsDNA levels and greater disease activity, suggesting that poor periodontal health or ongoing bacterial exposure may exacerbate lupus severity through systemic immune activation.9
In addition to xerostomia resulting from secondary Sjögren’s syndrome, medication-induced xerostomia can be a concern.1,7 Persistent xerostomia resulting from either increases the risk for dental caries, candidiasis, and mucosal discomfort.1,8
Specific medication risks include:
- Corticosteroids: For patients on long-term corticosteroid therapy, clinicians must also consider potential issues like adrenal suppression and delayed healing when planning invasive dental procedures.5,14
- Antimalarials: Drugs such as hydroxychloroquine can occasionally cause oral pigmentary changes, typically appearing as hyperpigmented macules most commonly located on the hard palate, buccal mucosa, and tongue.1 The medication also carries a risk of retinal toxicity.1,5
Given this complexity, a comprehensive medical history, including medication dosage, is essential during every dental assessment.
Management
A thorough clinical assessment requires an updated medical history that clearly documents autoimmune disorders, current medications, and systemic symptoms.4,5 For documenting mucosal findings, dental hygienists should note ulcer size, shape, location, duration, and associated discomfort.1,3 Intraoral photos are also valuable for monitoring progression and providing documentation for effective collaboration with other healthcare providers.1,4,5
Persistent, unexplained oral ulcers or discoid-like mucosal plaques warrant referral for biopsy and consultation with an oral surgeon or dermatologist, and follow-up with a rheumatologist after definitive diagnosis for management.3,4 The EULAR and ACR guidelines emphasize the importance of multidisciplinary management in lupus care.4,5 To ensure effective communication and collaboration with medical providers, information shared should include details on lesion characteristics, current medications, systemic manifestations, and recent laboratory findings if available.1,3-5
Given the association between exposure to A. actinomycetemcomitans and lupus activity, periodontal evaluation and, if necessary, collaboration with periodontists should be prioritized to reduce bacterial load, which may indirectly reduce systemic inflammation.9
Dental hygienists should provide education on daily oral hygiene strategies tailored to each patient’s symptoms.4,5 Recommendations may include the use of alcohol-free antimicrobial rinses, soft-bristled toothbrushes, and nonabrasive toothpaste formulations to minimize discomfort and mucosal irritation.8
Infection control must be proactively managed for immunocompromised individuals by ensuring strict adherence to standard infection control precautions.6,14 Collaboration between physicians and dental professionals is recommended to discuss risk-benefit analysis for delaying elective procedures during periods of heightened immunosuppression or when medication doses are elevated.4,5
In Closing
Dental hygienists are essential members of the interdisciplinary healthcare team that manages patients with lupus. Their ability to recognize early oral manifestations, assess medication effects, and implement patient-centered preventive strategies directly improves health outcomes. By maintaining awareness of oral manifestations of lupus, updating medical histories at each appointment, and collaborating with physicians and specialists, dental hygienists ensure comprehensive, evidence-based care for patients living with this complex autoimmune disease.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- García-Ríos, P., Pecci-Lloret, M.P., Oñate-Sánchez, R.E. Oral Manifestations of Systemic Lupus Erythematosus: A Systematic Review. Int J Environ Res Public Health. 2022; 19(19): 11910. https://pmc.ncbi.nlm.nih.gov/articles/PMC9565705/
- Crincoli, V., Piancino, M.G., Iannone, F., et al. Temporomandibular Disorders and Oral Features in Systemic Lupus Erythematosus Patients: An Observational Study of Symptoms and Signs. Int J Med Sci. 2020; 17(2): 153-160. https://pmc.ncbi.nlm.nih.gov/articles/PMC6990878/
- Manfredini, M., Pedroni, G., Bigi, L., et al. Acquired White Oral Lesions with Specific Patterns: Oral Lichen Planus and Lupus Erythematosus. Dermatol Pract Concept. 2021; 11(3): e2021074. https://pmc.ncbi.nlm.nih.gov/articles/PMC8172054/
- Aringer, M., Costenbader, K., Daikh, D., et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019; 71(9): 1400-1412. https://pmc.ncbi.nlm.nih.gov/articles/PMC6827566/
- 2025 American College of Rheumatology (ACR) Guideline for the Treatment of Systemic Lupus Erythematosus (SLE): Guideline Summary. (2025, May 7). American College of Rheumatology. https://assets.contentstack.io/v3/assets/bltee37abb6b278ab2c/bltec93920aad624e33/sle-guideline-summary-2025.pdf
- Hammad, R.N., Ahmad, S.A., Rasool, M.I. Impact of Biologic and Disease-Modifying Anti-Rheumatic Drug (DMARD) Therapies on Oral Health in Rheumatologic Patients: A Case-Control Study. Cureus. 2024; 16(11): e73179. https://pmc.ncbi.nlm.nih.gov/articles/PMC11624429/
- Pasoto, S.G., Adriano de Oliveira Martins, V., Bonfa, E. Sjögren’s Syndrome and Systemic Lupus Erythematosus: Links and Risks. Open Access Rheumatol. 2019; 11: 33-45. https://pmc.ncbi.nlm.nih.gov/articles/PMC6357904/
- Xerostomia (Dry Mouth). (2023, April 24). American Dental Association. https://www.ada.org/resources/ada-library/oral-health-topics/xerostomia
- Bagavant, H., Dunkleberger, M.L., Wolska, N., et al. Antibodies to Periodontogenic Bacteria Are Associated with Higher Disease Activity in Lupus Patients. Clin Exp Rheumatol. 2019; 37(1): 106-111. https://pmc.ncbi.nlm.nih.gov/articles/PMC6309750/
- Du, F., Qian, W., Zhang, X., et al. Prevalence of Oral Mucosal Lesions in Patients with Systemic Lupus Erythematosus: A Systematic Review and Meta-Analysis. BMC Oral Health. 2023; 23(1): 1030. https://pmc.ncbi.nlm.nih.gov/articles/PMC10734171/
- Abubakr, O.A., Youssef, A.M., Mohamed, M.A., Hamdy, M.A. Oral Mucosal and Dental Affection in Patients with Systemic Lupus Erythematosus: A Clinical Survey. Journal of Medicine in Scientific Research. 2023; 6(4): 1. https://jmisr.researchcommons.org/home/vol6/iss4/1/
- Rodsaward, P., Prueksrisakul, T., Deekajorndech, T., et al. Oral Ulcers in Juvenile-Onset Systemic Lupus Erythematosus: A Review of the Literature. Am J Clin Dermatol. 2017; 18(6): 755-762. https://pmc.ncbi.nlm.nih.gov/articles/PMC5680373/
- Ní Maolcatha, S., Nic Dhonncha, E., O’Connor, C., et al. The Lupus Band Test: A Review of the Sensitivity and Specificity in the Diagnosis of Lupus Erythematosus. Skin Health Dis. 2023; 3(4): e205. https://pmc.ncbi.nlm.nih.gov/articles/PMC10395624/
- Yasir, M., Goyal, A., Sonthalia, S. (2023, July 3). Corticosteroid Adverse Effects. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK531462/