Are you in need of CE credits? If so, check out our peer-reviewed, self-study CE courses here.
Test Your Oral-Systemic Link Knowledge
1. Which of the following oral pathogens induce platelet aggregation contributing to cardiovascular disease?
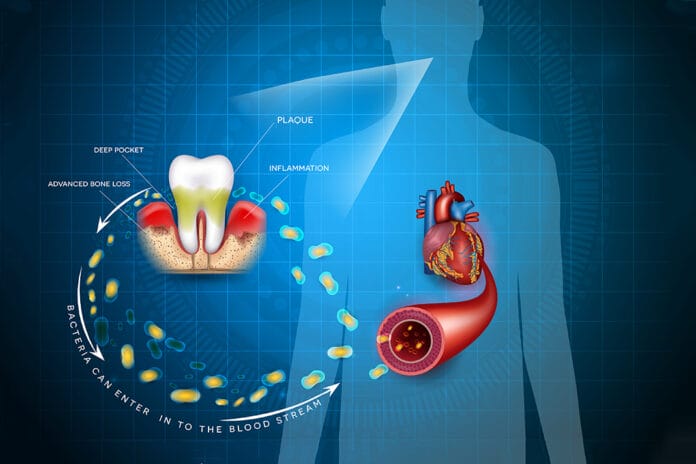
Multiple mechanisms contribute to the association between oral health and cardiovascular disease, including altered immune response, chronic inflammation, and platelet aggregation. Though many periodontal pathogens contribute to these conditions, only P. gingivalis was found to contribute to platelet aggregation.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
2. Patients with periodontitis are three times more likely to develop nosocomial pneumonia than those without periodontitis.
Nosocomial infections are acquired while receiving health care that was not present upon admission in health care facilities such as hospitals, long-term care facilities, or ambulatory settings.1
Multiple oral pathogens have been implicated in lung infections, including A. actinomycetemcomitans, A. israelii, Capnocytophaga spp, C. pneumoniae, E. corrodens, F. nucleatum, F. necrophorum, P. gingivalis, P. intermedia, and S. constellatus. Dental biofilm serves as a significant reservoir for pathogens to accumulate and spread to lower airways. For example, respiratory pathogens isolated from dental biofilm and lung fluid samples (bronchoalveolar lavage) from patients in intensive care units have been shown to be genetically the same. Individuals with periodontitis are three times more likely to develop nosocomial pneumonia compared to those that do not have periodontitis.2
1. Sikora, A., Zahra, F. (2023, April 27). Nosocomial Infections. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK559312/
2. Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
3. Which of the following inflammatory responses are associated with both Alzheimer's disease and periodontitis and is also considered the "hallmark" of Alzheimer's disease?
Complement activation, cytokine expression, and chemokine expression are all inflammatory processes associated with both periodontitis and Alzheimer's disease. However, only significant levels of inflammatory cytokines are the "hallmark" of Alzheimer's disease.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
4. Approximately what percent of pregnant women demonstrate clinical evidence of periodontal disease?
Due to significant hormone changes during pregnancy, pregnant women are more susceptible to gingivitis and periodontitis. Approximately 40% of pregnant women present with clinical evidence of periodontitis. Maternal infections, such as periodontitis, are associated with adverse pregnancy outcomes, including preterm labor, preterm or premature rupture of the membranes, pre-eclampsia, miscarriage, intra-uterine growth retardation, low birth weight, stillbirth, and neonatal sepsis.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
5. Diabetes mellitus and periodontitis have a bi-directional relationship in which one affects the other.
Diabetes mellitus and periodontitis have a bi-directional relationship in which one affects the other. Chronic infections, such as periodontitis, lead to exacerbated and dysregulated inflammatory responses, contributing to poor blood sugar metabolic control and increased insulin requirements.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
6. Bacterial pathogens, antigens, endotoxins, and pro-inflammatory cytokines produced during periodontal disease cannot cross the placental barrier. The cause of increased adverse pregnancy outcomes in mothers with periodontitis is completely unknown.
Bacterial pathogens, antigens, endotoxins, and pro-inflammatory cytokines produced during periodontal disease can cross the placental barrier. This results in disturbances in the maternal-fetal unit, possibly contributing to adverse pregnancy outcomes. F. nucleatum is the most common oral pathogen found in placental and fetal tissue.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
7. The periodontal pathogen P. gingivalis has been found in significantly elevated levels in patients with oral and esophageal squamous cell carcinomas. Additionally, periodontal disease has a positive correlation with pancreatic, colon, and lung cancers.
The periodontal pathogen P. gingivalis has been found in significantly elevated levels in patients with oral and esophageal squamous cell carcinomas compared to healthy patients. Research has shown that P. gingivalis and F. nucleatum stimulate tumorigenesis through direct interaction with oral epithelial cells, and the host's innate immune system mediates this effect. In oral squamous cell carcinoma, it has been shown that P. gingivalis, but not F. nucleatum, promotes invasion and metastasis of oral squamous cells by inducing matrix metalloproteinase 9 (pro-MMP9) expression.
This suggests that oral pathogens such as P. gingivalis and F. nucleatum could be biomarkers for the early stages of oral cancers and potential targets for prevention. Moreover, studies have found a positive correlation between periodontal pathogens and pancreatic, colon, and lung cancers.
Bui, F.Q., Almeida-da-Silva, C.L.C., Huynh, B., et al. Association between Periodontal Pathogens and Systemic Disease. Biomedical Journal. 2019; 42(1): 27-35. https://doi.org/10.1016/j.bj.2018.12.001
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.