Want to know how one amazingly energetic dental hygienist can produce $42,000 to $50,000 a month? Using time management and performing every task allowed under her state guidelines, this hygienist has created a superb daily flow. Assisted hygiene changed the trajectory of her career.

Patty Farmer, RDH, graduated from Prairie State College in 2002. Her LinkedIn account reveals a vast arena of dental experience, ranging from clinical to recruiting. “My passion is dentistry in all aspects: clinical, education, sales, management, and networking. I strive to find ways to advance our profession as a whole while also working to motivate individuals in the dental field to move beyond their self-deemed limitations.”
Many have reached out and asked Patty how she manages to accomplish so much, so well, and so stress-free. Here is her advice on assisted hygiene scheduling.
Study the Doctor
First, get to know your doctor. “Spend time learning your dentist and how they diagnose.” Work together on radiographs and patient exams so you can become intuitive and make notes of suspicious areas to go over during the doctor examination. Have your doctor feel and see what you find suspicious during the appointment’s clinical portion to help build that trust. Assisted hygiene is an overall team care approach, so working together is essential for patient flow and care.
While assisted hygiene sounds scary, Patty believes that she has more actual treatment time with the patient. Assisted hygiene means no operatory set up, clean up, or instrument processing duties for the hygienist unless there is a natural break in the schedule.
The assistant exposes any necessary radiographs, updates health history, questions the patient for any potential issues, administers the pre-procedural rinse, and explains all the new updated COVID-19 protocols. All this takes approximately 15 minutes of the hygiene assistant’s time.
The hygienist then conducts treatment for approximately the next 30 minutes. This time is used to establish a relationship, basic pleasantries, review exposed radiographs, bacterial laser reduction as needed, probe as the assistant records the measurements, ultrasonic scale as needed (less now with the pandemic protocols), hand scale, and then hygiene examination.
The exam is at the appointment’s completion as it is easier to visualize areas of suspicion after each interproximal area has been debrided so that potential lesions may have been noticed. Attention is paid to any shadowing or cracks on teeth, and oral hygiene instructions are performed during scaling. Polishing is done by either the hygienist or in states allowing, and with the appropriate certification, the hygiene assistant may polish.
Notes are taken and left for the doctor for use during the patient examination. The hygienist then leaves the patient and moves on to the next pre-set treatment room with the patient already seated and ready.
The assistant remains in the operatory, along with the doctor, for the previous patient’s examination. Should any questions arise from the notes, the assistant can go between the operatories to clarify. The assistant then schedules the next recare appointment, applies fluoride, and provides any products being dispensed before dismissing the patient to the front desk as needed. The assistant then breaks down the operatory, resets, runs the instruments, and seats the next patient.
The Team and Time Management
In order to make assisted hygiene flow, the most important aspect is a team approach to time management. A daily morning huddle helps prepare the day’s game plan. Multiple operatories are also essential. Following the 15-minute assistant, 30-minute hygiene, 15-minute assistant time frame allows for exceptional patient care and the ability to treat significantly more patients per day.
Flexibility in the game plan is essential. Treatment needs may vary throughout the day, and the goal is to complete needed treatment the same day whenever possible. These additions may be more in-depth cancer screenings, sealants, periodontal treatment plans, salivary testing, or perhaps additional radiographs. Ultimately, all possible diagnostics will be accomplished the same day rather than being reappointed, and only periodontal therapies and restorative will be rescheduled.
Patty says patient flow is better “with ease of additional hands to collect materials and reduce needs for the dental hygienist to stop and start while treating the patient. This allows patients to have care needed, rather than reappoint and “consume” more of the schedule. It’s all about time management!”
Same-day treatment saves the patient time and increases their perception of the office, saves office time and money by not reappointing and using more PPE, and more chair time in setup and break down. Everything with assisted hygiene is about time management, and this flexibility of treatment is just one more example.
Many choosing to work an assisted hygiene schedule report feeling more support during the workday as the treatment responsibilities are clearly laid out, and a designated assistant keeps the room flow manageable. The team approach creates a camaraderie of respect for all team members and ownership of the schedule.
The question of compensation is always an issue and a very personal decision. Assisted hygiene can be harder on your body with increased scaling, and long-term implementation depends on excellent ergonomics. Because production is exponentially increased, it stands to reason that compensation should be increased. Patty states that some hygienists will choose a higher base salary, some choose production percentage only, but it appears that most will be hourly salary plus a percentage of production (not collections).
Assisted dental hygiene during the current pandemic created some changes in patient flow. Please follow your specific state protocols. Below are the recent changes Patty has made in Illinois to follow guidelines:
1. Patient is prescreened over the phone or via the patient communication system prior to the day of the appointment. Patients who are over 65, immune-compromised, or with existing respiratory or heart concerns should be considered to hold off on nonemergent dental procedures until a space with minimal contamination concerns can be provided. There is a potential to limit these patients to each day’s first appointment to help minimize risk from others.
2. At the beginning of the day, the hygiene department should huddle to review potential struggles to be handled with the day and work together for a plan to keep it as smooth as possible.
3. Upon arrival for visit, the patient should call/text into the practice system that they have arrived and remain in their vehicle until a room is available to seat them for treatment. Upon entering practice (or just outside the front door), the patient will have temperature logged. Temps over 100.4°F will be reappointed immediately. The practice will decide if this is done by assistant or office staff
4. Before seating the patient, the assistant will have the patient wash hands or use hand sanitizer and rinse with a preoperative rinse for 30 seconds. The rinse is again used mid- and post-treatment dispensed by the hygienist.
5. Paperwork to update medical/dental history, BP, and needed radiographs taken by an assistant.
The hygienist may need to activate radiograph button to allow the assistant to move the recommended six-foot distance from the beam yet not exit the op with PPE on.
6. Assistant is to remain in the operatory at the beginning of hygiene treatment for any help taking records such as perio charting and intraoral photos needed.
7. Assistant will leave PPE (gown and “top mask” if using to expand the life of an N95 respirator) in the op to potentially be reused at the end of the appointment and for operatory clean up.
8. Hygienist will commence with treatment/OHI, make a list of any areas of concern for treatment to expedite exam for the doctor, and reappoint for hygiene follow-up (if time allows, otherwise completed with assistant after completion of doctor exam).
9. During hygiene treatment, the assistant will prepare the next hygiene operatory and work on sterilization. Clean/new PPE is used on the “clean side” of the sterilization area when removing instruments from the sterilizer. Best to time this activity with changing PPE before stepping into an op for set up. A hook has been adhered to the wall just inside each operatory for that appointment’s PPE. When leaving the operatory, the gown, shield, and over-mask is placed on the hook to be used only with that patient. Gown and mask are wrapped in the patient headrest cover and disposed of at the end of the appointment. The shield is wiped down and set with the fresh PPE for the next appointment in that operatory.
10. With the assistant working with two hygienists, a 20-minute appointment stagger should be in place to allow the assistant to complete the first hygienist appointment.
11. Depending on time constraints to schedule and if the assistant is certified, patients should be polished by the assistant to allow the hygienist to move forward in the schedule, maintaining time respect for patients.
12. Upon return to the operatory, the assistant will reuse necessary PPE left from the beginning of the appointment to complete the doctor exam through excusing the patient and sanitizing the operatory.
13. After the hygiene exam completed with the doctor, the assistant may offer fluoride treatment to the patient prior to escorting the patient out of the operatory.
Patty’s Additional Elements to Consider
During the pandemic, appointments have been extended to 45 minutes (30 minutes only if families already in the same “bubble”). Average patients seen during the pandemic is 11-12 per day.
-Be sure that scheduled appointments are set for all treatments needed/expected for each appointment, including radiographs, perio charting, LBR, and/or need for IO photos if known in advance.
-When pre-scheduling, increase appointment time if additional services will be scheduled, such as laser or advanced cancer screenings. Note this on the appointment to help with treatment flow.
-When the hygienist has additional time available and various tasks completed (sharpening instruments, for example), an effort is to be made to assist any areas in need of attention for the hygiene department as a team, including tasks that the assistant may have fallen behind on. Assisted hygiene runs best when everyone works as a complete unit for a single goal.
-If possible, have product bags prepared ahead of time to dispense to patients, keep time management goals, and to reduce additional exposure to the supplies when going through the drawers after treatment.
-Due to current pandemic concerns, the hygienist needs proper HVE ability during ultrasonic use without an assistant to reduce the aerosol spread in the operatory.
-Should any questions arise with home care clarification or treatment needs by the patient, the assistant should be trained in treatment explanation, treatment options available, and home care instructions for the patient to aid in education. This helps to solidify the hygiene department team in that patients will obtain a consistent message throughout care.
The schedule below is an example of a system involving one hygienist and one assistant:
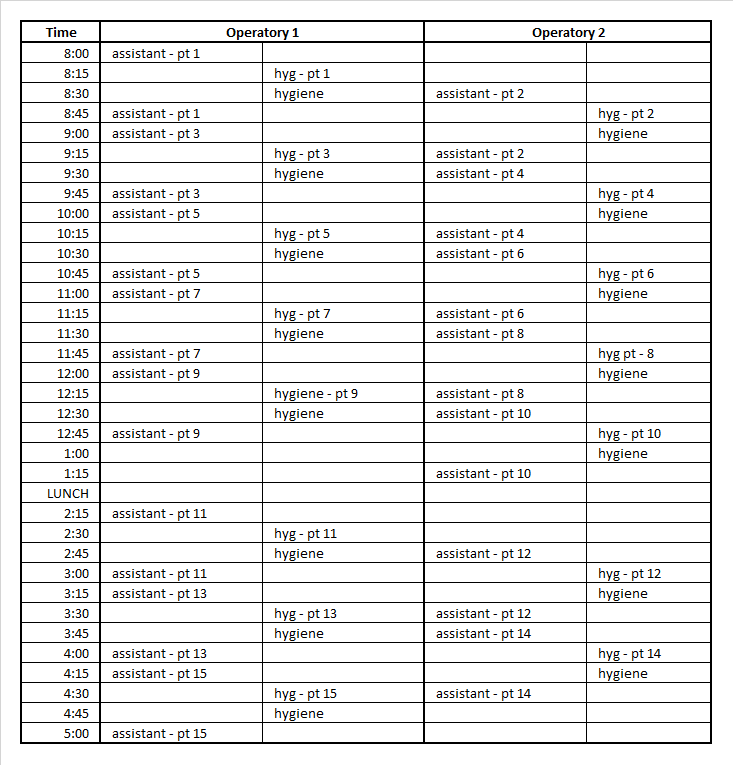
Patty’s Notes about Her Suggested Schedule
-This is a very basic outline and not static as to who is where always. It is a team approach; the assistant maybe cleaning a room and hygiene is starting with radiographs or finishing fluoride treatment. Both assistant and hygienist work together seamlessly to enhance patient flow and appointment management.
-New patients are given 75-minute appointment times hygiene time with an assistant as needed.
-SRP is given one-hour of hygiene time.
-Perio maintenance receive 45 minutes of hygiene time.
-Knowing the patient and what the needs are for recare appointments may require adjusting the time scheduled.
-Not all patients get radiographs or need full 15 minutes of assistant time, so the assistant needs to be more fluid between rooms and the sterilization area.
-The doctor will often pop in and do exams two at a time, especially when it is a family, which frees him/her up for a full hour.
-Sometimes, radiographs or full perio charting are done at the end of the appointment, depending on the day’s flow.
-This can be very fluid dance-like, and the morning huddle is crucial to game planning day.
Patty loves the team approach to patient care and truly feels that her patients receive the best care. Patty is a superhero in her office and laughingly says she “covers more ground faster with a sidekick than alone.”












