Are you in need of CE credits? If so, check out our peer-reviewed, self-study CE courses here.
Test Your Trismus Knowledge
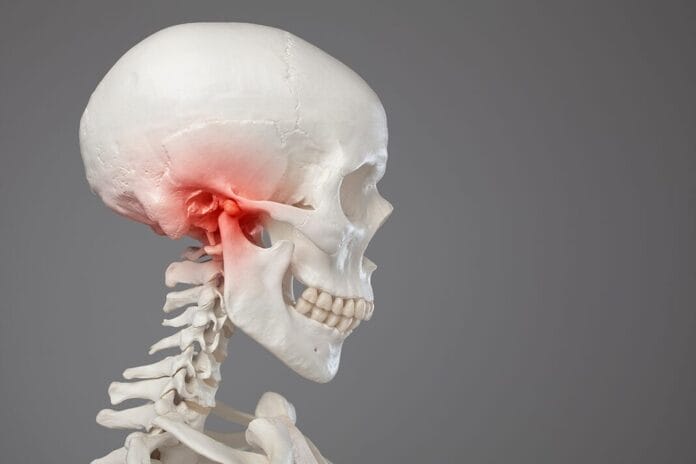
1. Trismus is the restriction of the range of motion of the jaw. It was initially described as a symptom of tetanus.
Trismus is the restriction of the range of motion of the jaw. The normal range of motion when opening the mouth is 40 to 60 mm. A limited range of opening that is less than 35 mm is indicative of trismus.1
Trismus was initially described in patients with tetanus. However, currently, it refers to restricted mouth opening due to any etiology.1
In most cases, trismus is a temporary condition that resolves within two weeks. However, it can be permanent in some cases and interfere with everyday activities, such as speaking, eating, swallowing, and maintaining proper oral hygiene. Aspiration due to impaired swallowing mechanisms has also been associated with trismus.1
Reference
1. Santiago-Rosado, L.M., Lewison, C.S. (2022, October 22). Trismus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493203/
2. Which of the following can be an etiological factor or cause of trismus?
Multiple conditions can result in the development of trismus. Acute trismus can be caused by facial, mandibular, or iatrogenic trauma. Chronic trismus is often associated with temporomandibular disorder (TMD), malignant neoplasia, complications from surgery, radiotherapy for head and neck cancer, local infections, and connective tissue disorders. Severe trauma can also cause chronic trismus.1
Reference
1. Santiago-Rosado, L.M., Lewison, C.S. (2022, October 22). Trismus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493203/
3. Trismus can be a complication of the administration of local anesthesia.
Trismus can be a complication of the administration of local anesthesia, such as the penetration and deposition of anesthetic into the masticatory muscles. For example, if the tip of the needle becomes barbed during the administration of an inferior alveolar nerve block (IANB), it may tear the medial pterygoid muscle upon withdrawal, leading to muscle spasm and trismus. Repeated muscle punctures within a short period of time in the same area or an incorrectly administered IANB or posterior maxillary injection may also cause trismus.1
Additionally, injury to the inferior alveolar artery or vein may lead to a hematoma in the pterygomandibular space, resulting in trismus.1
Tissue expansion due to large quantities of local anesthetic solution deposited into a restricted region, and the local anesthetic itself, can be contributing factors to trismus.1
Delayed onset trismus, typically appearing two to three days after an injection, is frequently attributable to a needle-track infection.1
Reference
1. Khalifeh. B., Simonian, K., Houmani, M., et al. Trismus Following Inferior Alveolar Nerve Block: A Case Report. Cureus. 2024; 16(11): e73394. https://pmc.ncbi.nlm.nih.gov/articles/PMC11630894/
4. Which of the following is not typically considered a potential sign of trismus-related malignant neoplasm?
Trismus rarely presents as the primary sign of malignant neoplasms, yet malignant neoplasms should not be ruled out when patients present with unexplained trismus. Cases of misdiagnosis of trismus related to TMD have led to delayed diagnosis and treatment of malignant neoplasms.1
If the patient presents with the following five signs and symptoms, referral to a specialist should be considered:1
- Opening less than 15 mm
- No history of TMJ clicking
- Pain of non-myofascial origin or neuralgia-associated pain
- Lymphadenopathy (swollen lymph nodes)
- Suspicious intraoral soft tissue lesions
The primary sites of malignant neoplasms that induce trismus include:2
- Tongue
- Maxillary sinus
- Nasopharynx
- Retromolar trigones
- Infratemporal fossa
- Nasal cavity
- Hypopharynx
- Cervical esophagus
- Parotid gland
- Floor of the mouth
- Buccal mucosa
- Larynx
- Oropharynx
- Thyroid
- Palate
- Ear
- Submandibular gland
References
1. Santiago-Rosado, L.M., Lewison, C.S. (2022, October 22). Trismus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493203/
2. Raj, R., Thankappan, K., Janakiram, C., et al. Etiopathogenesis of Trismus in Patients with Head and Neck Cancer: An Exploratory Literature Review. Craniomaxillofac Trauma Reconstr. 2020; 13(3): 219-225. https://pmc.ncbi.nlm.nih.gov/articles/PMC7797966/
5. Radiotherapy for head and neck cancer can cause fibrosis of the muscles of mastication, leading to trismus. The risk of trismus increases when the deep layer of the masseter muscle is in the radiation zone.
A common complication of head and neck cancer treatment is trismus, with an estimated 38% to 42% of patients being affected. Surgical procedures can scar the mastication muscles and restrict mandibular opening. Radiotherapy can cause fibrosis of the muscles of mastication, leading to the development of trismus. The risk increases if the median pterygoid muscle is in the radiation zone.1
Radiotherapy can damage tissues in two ways, contributing to the onset of trismus, either directly from DNA damage or indirectly through reactive oxygen species (ROS). Over time, the body tries to repair the damage via increased collagen production. The buildup of collagen reduces blood flow, leading to stiff, poorly functioning tissue and, in some severe cases, necrosis.2
References
1. Santiago-Rosado, L.M., Lewison, C.S. (2022, October 22). Trismus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493203/
2. Raj, R., Thankappan, K., Janakiram, C., et al. Etiopathogenesis of Trismus in Patients with Head and Neck Cancer: An Exploratory Literature Review. Craniomaxillofac Trauma Reconstr. 2020; 13(3): 219-225. https://pmc.ncbi.nlm.nih.gov/articles/PMC7797966/
6. Treatment of trismus depends on the cause, but is primarily treated symptomatically.
Treatment of trismus depends on the cause, but is primarily treated symptomatically. Symptom-directed interventions include heat therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants in the acute phase. A soft diet should also be encouraged for the duration of the symptoms.1
If symptoms of post-traumatic or post-operative trismus persist for longer than a week, physiotherapy may help. Physical therapy consists of exercises to open the mouth against applied resistance and opening and closing the mouth, including lateral movements. Chewing sugar-free gum to stimulate lateral movements may also be indicated.1
Physiotherapy aims to alleviate edema and fibrosis, restore blood circulation, and improve range of motion and muscle strength. It also keeps the muscles active, which could prevent chronic trismus.1
When trismus becomes chronic due to fibrosis or ongoing radiotherapy, it may require more intensive physiotherapy. This can involve specialized jaw motion rehabilitation devices or microcurrent therapy, especially for patients who haven't responded to conservative treatments.1
In extreme cases of trismus or for patients who repeatedly haven’t responded to conservative treatments, referral to a maxillofacial surgeon may be necessary because they may require surgical intervention. Multiple surgical interventions have been utilized to improve function, including reducing the mandibular height to achieve a larger mouth opening, coronoidectomy, or tissue release and free flap reconstruction.1
Reference
1. Santiago-Rosado, L.M., Lewison, C.S. (2022, October 22). Trismus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493203/