The thyroid secretes certain hormones that are active participants in different systems of the body. The thyroid affects many parts of the body, including metabolism, hormones, body temperature, and it keeps the brain, heart, muscles, and other organs healthy. When too many or too few hormones are produced from the thyroid, it’s considered a thyroid disorder.1
Dental concerns about thyroid medications are reviewed below. The dental hygienist can also review dental management strategies for treating patients with thyroid conditions. It should be pointed out that dental professionals are likely treating patients who are unaware of their thyroid disorders.
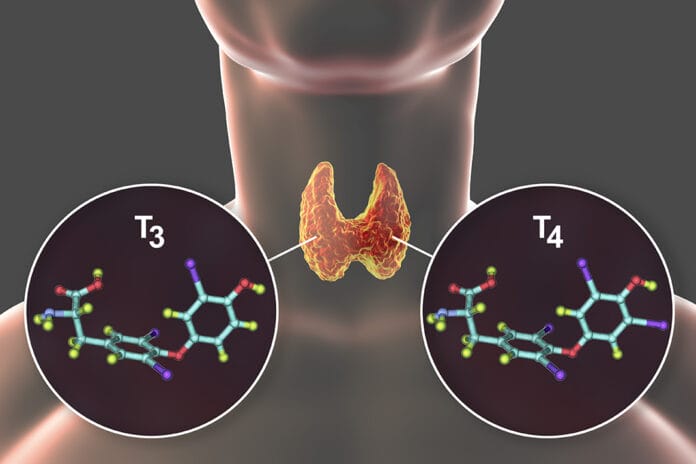
The two main conditions of thyroid disorders are hypothyroidism and hyperthyroidism. The thyroid controls the metabolism, specifically with the hormones T3 (triiodothyronine), the active form, and T4 (thyroxine), the storage form.
When the thyroid works properly, it maintains the right amount of hormones in keeping the metabolism and other body functions working successfully. As the hormones are used, the thyroid will release replacements. When this doesn’t happen, then other means, including synthetic thyroid hormones and antithyroid treatments, are needed.1,2
Thyroid Hormones and Tests
A thyroid test is a blood test to check hormone levels. Since thyroid hormones in the blood are bound by protein, a small portion is free to enter tissues to have a biological effect. Thyroid tests measure the total protein-bound and free hormone levels.3
- Triiodothyronine (T3): Accounts for 5% of thyroid hormone circulating in the blood. A normal total T3 level ranges from 80 to 220 ng/dL. T3 has four times the strength of T4.3
- Thyroxine (T4): This is the primary form of thyroid hormone, and about 95% circulates in the blood. T4 is the storage hormone, and by losing an iodine atom, it’s converted to T3, the active hormone to be used by the cells. This conversion happens mainly in the liver and specific tissues, including the brain. A normal T4 level ranges from 5.0 to 12.0 ug/dL.3,4
- Thyroid-stimulating hormone (TSH): The pituitary gland controls the thyroid gland and releases TSH into the blood to trigger the thyroid to make more hormones. This process works as needed, and if the pituitary gland senses a low level of thyroid hormones, it produces more TSH to stimulate the thyroid gland to produce more hormone. If there are too many thyroid hormones, then the pituitary gland slows down production.3
- A high TSH level indicates the thyroid gland is not producing a sufficient number of hormones and results in hypothyroidism, while a low TSH level implies hyperthyroidism. Normal TSH values are 0.5-5.0mIU/L.3
Treatments for Thyroid Conditions
Thyroiditis ─ Thyroiditis is inflammation or swelling of the thyroid gland and can progress into under or over-production of the thyroid hormones. It occurs in three phases. The hyperthyroidism stage is usually short-term (about one to three months) and is when the abundance of stored thyroid hormones is released from the damaged cells. Following the excessive release of thyroid hormones, the more common hypothyroidism phase occurs by the opposite effect of a decrease in the thyroid production of hormones. This phase is long-lasting and can become permanent.
The euthyroid phase is the return to a normal phase when either between the hyper and hypo phases or after the inflammation has subsided and recovery has happened to return to normal hormone levels.5
Hyperthyroidism
Hyperthyroidism, also called thyrotoxicosis, is an overactive thyroid. When the thyroid makes too much of the hormones T3 and T4, the body uses energy too quickly. This results in fatigue, weight loss, fast heartbeat, high blood pressure, nervousness, mood swings, intolerance to heat, trouble sleeping, irregular menstrual cycles, and diarrhea. Noticeable physical signs are protruding eyes, goiter, and shaky hands.6
Some causes of hyperthyroidism may be from family histories, such as Graves’ disease, thyroiditis, nodules on the thyroid, and excess iodine.1 In the United States, about 1.2% or one out of 100 people have hyperthyroidism.6
Graves’ disease ─ Graves’ disease is the most common cause of hyperthyroidism, and it’s an autoimmune disorder that attacks the thyroid and causes it to make too many thyroid hormones. The treatment for Graves’ disease is to cease producing thyroid hormones and block the effect of the hormones on the body.
People with Graves’ disease should avoid iodine foods or supplements as it will make hyperthyroidism worse. Blood tests will show low TSH and high T3 and T4.7
Thyroid Storm ─ Thyroid storm is a rare, life-threatening condition with hyperthyroidism that occurs when untreated, undertreated, severe infection, or medical stressors are apparent. Complications may be high fever, dehydration, rapid and irregular heart rate, heart failure, weakness, vomiting, diarrhea, and disorientation.
If swift, aggressive treatment isn’t initiated, it can be fatal, and the mortality rate may be up to 75%. The primary treatment is to decrease the circulating thyroid hormone levels and to decrease production.8
Radioactive iodine is a common and effective treatment for hyperthyroidism. The thyroid requires iodine to produce hormones, and radioactive iodine is taken orally either by capsule or liquid. The radioactive iodine enters the thyroid cells and slowly destroys the overactive thyroid cells, resulting in a smaller thyroid causing fewer symptoms.
A benefit of this treatment is that it does not affect other body tissues. A negative is that many people will eventually develop hypothyroidism since the thyroid-producing cells have been destroyed. It’s been recognized that hypothyroidism is easier to treat for long-term health than hyperthyroidism.7,9
Hyperthyroidism Medications
Hyperthyroidism medications are prescribed to level out the hormones to a normal status. The thyroid condition dictates which medication is better suited for the patient.
Antithyroid medications: They are not a cure but are determined to be the simplest way to treat hyperthyroidism. They work slowly by taking a few weeks for effect by decreasing or inhibiting the number of hormones produced from the thyroid. As these medications do not cause permanent damage, the symptoms will return once the medications are stopped, so it’s recommended to seek more permanent treatments.10
- Methimazole (Tapazole): This is the preferred antithyroid medication. Methimazole blocks the thyroid from using iodine which aids in producing the thyroid hormones. Methimazole has fewer side effects and reverses hyperthyroidism sooner than PTU. This medication is taken once a day.4
- Propylthiouracil (PTU): Inhibits the thyroid gland from using iodine to help slow the overproduction of thyroid hormones while blocking the conversion of T4 to T3. It’s quickly absorbed and is extensively metabolized, causing a short-acting timespan and relying on patients to take this medication two to three times a day. Although PTU has more side effects than other thyroid medications, it is the preferred choice for hyperthyroidism in early pregnancy, severe thyroid storm, and in the case of serious side effects caused by methimazole.4
Side effects of antithyroid medications: Rash, upset stomach, drowsiness, sore throat, chills, fever, jaundice, liver disease, and decreased white blood cells.10
Precautions and interactions for antithyroid medications: Vaccinations, alcohol, beta-blockers, warfarin, digoxin, theophylline, sodium iodide, liver disease, selective serotonin reuptake inhibitors (SSRIs), oral diabetics, and insulin.11
Dental concerns with antithyroid medications: Bitter aftertaste, mouth sores, sore throat, infections, swollen salivary glands, and loss of taste.10,11
Beta-blockers: Beta-blockers do not block the production of the hormones; they only control the symptoms until other treatments take effect.1 They act quickly to relieve symptoms such as tremors, rapid heartbeat, heat intolerance, sweating, diarrhea, muscle weakness, and nervousness.9
Beta-blockers would be recommended for hyperthyroidism when:
- An occurrence of a very high resting heart rate or high blood pressure
- The inability to tolerate an antithyroid medication
- Subacute thyroiditis
- The receiving or planning of radioactive iodine treatment
- Propranolol: Is the preferred beta-blocker as it has a more direct effect on hypermetabolism
- Atenolol: Is the second most common beta-blocker used with hyperthyroidism and Graves’ disease; it helps decrease the resting heart rate, high blood pressure, and angina
- Metoprolol: It is sometimes used to treat hyperthyroidism symptoms but mainly to treats angina and high blood pressure.
- Acebutolol: May be prescribed but is less common for hyperthyroidism12
Hypothyroidism
Hypothyroidism occurs from an underactive thyroid, and the thyroid produces too few hormones (T3 and T4) to be released into the bloodstream and slowing down the metabolism. The body doesn’t use up energy properly. This results in fatigue, weight gain, dry, coarse thinning hair, memory loss, dry, rough skin, heavy and frequent menstrual cycles, hoarse voice, inability to tolerate cold temperatures, puffy face, fertility issues, slowed heart rate, goiter, hair loss on the outer third of the eyebrow, and constipation.1
Hypothyroid occurrences are by injury, radiation, medications, thyroid gland removal, thyroiditis, or congenital. In the United States, about 4.6% or five out of 100 people have hypothyroidism.
Hashimoto’s thyroiditis ─ Hashimoto’s thyroiditis is the most common form of hypothyroidism. This is an autoimmune condition when the body’s cells attack and damage the thyroid. Hashimoto’s thyroiditis will develop slowly over time as the thyroid gland becomes more damaged and less functional. Although it isn’t curable, the condition is highly treatable with lifelong thyroid hormone replacement medications. Blood tests will show a high TSH level meaning the thyroid is not producing enough T4.1
Myxedema Coma ─ Myxedema coma, also called myxedema crisis, occurs when hypothyroidism is at its most complicated stage when left untreated, unrecognized, and undiagnosed. Hormone levels become extremely low, and the body’s functioning slows to the severity of a life-threatening medical emergency.14
Hypothyroidism Medications
Hypothyroidism medications are synthetic or natural forms of T3 and T4. Taking medications will require regular monitoring to make sure the hormone levels are maintaining. These medications last in the body for a long time, so a single daily dosage is usually taken in the morning at the same time every day without food (food can slow the absorption, and fasting quickens the absorption).10
Synthetic and natural thyroid medications ─ Both are made in labs and meet the federal regulations and guidelines. They contain consistent amounts of thyroid and are prescribed in different strengths.15
The synthetic medication is made from levothyroxine sodium, and most contain the hormones T3, T4, or both. The medications are prescribed in accordance with age, gender, and body weight. There are many doses available.15
The natural medication is derived from an animals’ desiccated thyroid, such as a cow or sheep but more commonly pig. The starting dose is 30 mg, with adjustments as needed in 15 mg doses.15 GDRX)
Levothyroxine (Synthroid, Levoxine, Unithroid, Tirosint), often referred to as L thyroxine, levo T, levothroid: Levothyroxine is prescribed to treat hypothyroidism and comes in an oral and injectable form. It is the synthetic form of the hormone T4 and the medication of choice for hypothyroidism. It is FDA-approved.16
Side effects: Joint and chest pain, anxiety, palpitations, mood changes, choking sensation, heat intolerance, hair and weight loss, decreased bone density, shortness of breath, insomnia, headaches, cramps, and diarrhea.16
Precautions and interactions: Iron and calcium supplements, aluminum hydroxide (in some antacids), soy, high fiber diets, oral contraceptives, estrogen, testosterone, antidepressants, antiseizure, and statins.10,16
Dental concerns: Difficulty swallowing, difficulty breathing, fainting, swelling of the lips, throat, and tongue, jaw and neck pain, and trouble sitting still.17
Liothyronine (Cytomel, Triostat) ─ Liothyronine is the synthetic form of T3. It is not commonly prescribed for straight hypothyroidism but in thyroid disorders such as goiters or in addition with thyroid cancer therapy. The recommended dosage depends on the condition being treated and the level of thyroid dysfunction. Proper dosing is challenging as the normal ratio of T3 to T4 is generally 16:1. It’s short-acting and requires a split dosage twice a day.18
Side effects of liothyronine: Weak or shallow breathing, confusion, feeling hot or cold, chest pressure to jaw or shoulder, weight loss, increased appetite, light-headed, headaches, dizziness, vision problems, seizures.18
Precautions and interactions for liothyronine: Cholesterol medications, birth control, antidepressants, steroids, blood thinners, cough or cold medicines, insulin or oral diabetes medications, multivitamins with minerals, and not to be used to treat weight problems.18
Dental concerns of liothyronine: Difficulty breathing, increased blood pressure, jaw pain, trouble sitting still, and dizziness.18
Natural (natural source) Desiccated (dried) Thyroid (hormone) ─ Natural desiccated thyroid drugs are also referred to as NDT, natural thyroid, or porcine thyroid. The medication is derived from the dried thyroid gland of animals, commonly pigs. These medications work by replacing hormones that the thyroid can no longer produce, such as T3 and T4. These medications are not commonly prescribed as they are a combination medication of T3 and T4 and may not contain a sufficient ratio. This can induce elevated T3 levels, leading to side effects. Although certain select patients may respond very well to NDT, Synthroid is usually tried first. T3 absorption from NDT’s peak is four to eight hours and will require doses up to three times a day.4
Armour Thyroid, NP Thyroid, Nature-Throid, Westhroid: Armour Thyroid is the most commonly prescribed of the natural thyroids. Derived from desiccated pig thyroid, it is a mix of both hormones T3 and T4. There are minimal clinical trials and has not been approved by the FDA.15
Side effects of NDT: Lack or increased appetite, hot flashes, leg cramps, mood changes, menstrual cycle change, muscle weakness, headaches, vomiting, tremors, and shallow breathing.
Drug interactions and precautions for NDT: Testosterone, estrogen, birth control, salicylates, sucralfate/antacids, omeprazole, blood thinners, oral diabetes, insulin, digoxin, oral steroids, and iron.19
Dental concerns of NDT: None.
Oral Health Concerns
An article titled “Oral manifestations of thyroid disorders and its management” provided two tables regarding related oral health concerns: the authors, Drs. Shalu Chandna and Manish Bathla drew attention to the oral health conditions listed below.
Hypothyroidism:
- Salivary gland enlargement
- Compromised periodontal health – delayed bone resorption.
- Macroglossia
- Glossitis
- Dysgeusia
- Delayed dental eruption
- Enamel hypoplasia in both dentitions: less severe in the permanent dentition
- Micrognathia
- Thick lips
- Mouth breathing20
Hyperthyroidism:
- Increased susceptibility to caries and periodontal disease
- Burning mouth syndrome
- Enlargement of extra glandular thyroid tissue
- Maxillary and mandibular osteoporosis
- Accelerated dental eruption
- Development of connective tissue diseases such as systemic lupus erythematosus and Sjogren’s syndrome20
Dental Management
Drs. Chandna and Bathla suggested the following considerations for dental patients with thyroid conditions:
- Thyroid patients may be more susceptible to infection due to delayed healing from a decreased metabolic activity in fibroblasts.
- PTU medication has anti-vitamin K activity which can promote excess bleeding, increasing the risk of hemorrhaging.
- Although rare, methimazole can cause agranulocytosis’s rare reaction to increase susceptibility to oral infections and promote weak wound healing.
- Patients with hyperthyroidism may have increased anxiety and stress, which can be triggered during stressful dental appointments that may cause a thyroid storm.
- Epinephrine is contraindicated.
- Hyperthyroidism patients may have elevated blood pressure and heart rate.
- Aspirin is contraindicated as it interferes with the protein binding of T3 and T4 by increasing their free form and worsening symptoms of hyperthyroidism.20
- Using a thyroid collar when exposing radiographs, as the thyroid is extremely sensitive to radiation exposure.
Fluoride
The thyroid gland is one of the most fluoride-sensitive tissues in the body. Fluoride was previously used to treat hyperthyroidism because it reduces thyroid activity by mimicking the action of TSH. Iodine and fluorine are both parts of the halogen group of atoms, making them antagonistic. Excessive fluoride correlates with an iodine deficiency causing a disruption of the thyroid gland. This process enhances the effects of an increase in TSH and a decrease in T3 and T4, which causes hypothyroidism. With a vulnerable thyroid gland and fluoride exposure, it can suppress the thyroid gland’s function by suppressing and diminishing TSH levels.20
In Closing
According to the American Thyroid Association, an estimated 20 million Americans have some form of thyroid disease, and up to 60 percent are unaware they have a thyroid condition.21 With these numbers, we are bound to treat many patients who are unaware of a possible thyroid condition. Knowing the symptoms orally and systemically may help identify a thyroid issue and improve a patient’s quality of life.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Thyroid Disease. (2020, April 19). Cleveland Clinic. Retrieved from https://my.clevelandclinic.org/health/diseases/8541-thyroid-disease
- Hyperthyroidism (Overactive Thyroid). (2020, November 14). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659
- What Are Normal Thyroid Hormone Levels? (n.d.). UCLA Health. Retrieved from https://www.uclahealth.org/endocrine-center/normal-thyroid-hormone-levels
- Shomon, M. (2020, August 22). Medications Used to Treat Thyroid Disease. Very Well Health. Retrieved from https://www.verywellhealth.com/thyroid-disease-medications-3231845
- (2018, October 26). Cleveland Clinic. Retrieved from https://my.clevelandclinic.org/health/diseases/15455-thyroiditis
- Hyperthyroidism (Overactive Thyroid). (2016, August). National Institute of Health. Retrieved from https://www.niddk.nih.gov/health-information/endocrine-diseases/hyperthyroidism
- Graves’ Disease. (2017, September). National Institute of Health. Retrieved from https://www.healthline.com/health/thyroid-storm
- Moore, K. (2018, September 28). Thyroid Storm. Retrieved from https://www.healthline.com/health/thyroid-storm
- Graves’ Disease. (2020, December 05). Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/graves-disease/diagnosis-treatment/drc-20356245
- Thyroid Medications. (n.d.). John Hopkins Medicine. Retrieved from https://www.hopkinslupus.org/lupus-treatment/common-medications-conditions/thyroid-medications/
- Antithyroid Agent. (2021, March 3). com Retrieved from https://www.drugs.com/cons/antithyroid-agent-oral-rectal.html
- Beta Blockers and Hyperthyroidism: Side Effects and Natural Alternatives. (2018, June 18). Natural Endocrine Solutions. Retrieved from https://www.naturalendocrinesolutions.com/articles/beta-blockers-and-hyperthyroidism-side-effects-and-natural-alternatives/#
- Hypothyroidism (Underactive Thyroid). (2016, August). National Institutes of Health. Retrieved from https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism
- Basina, M. (2021, January 26). What is Myxedema Coma? Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/myxedema-coma#other-causes
- Armitage, M. (2020, April 17). Natural (Armour Thyroid) vs Synthetic (Synthroid) Thyroid Medication: Which One Is Right for Me? Good Rx. Retrieved from https://www.goodrx.com/blog/armour-thyroid-vs-synthroid-dosing-cost-side-effects/
- (n.d.). RxList. Retrieved from https://www.rxlist.com/consumer_levothyroxine/drugs-condition.htm
- Levothyroxine Side Effects. (2020, August 17). com. Retrieved from https://www.drugs.com/sfx/levothyroxine-side-effects.html
- Liothyronine Side Effects. (2020, August 28). com. Retrieved from https://www.drugs.com/sfx/liothyronine-side-effects.html
- Slowiczek, L. (2018, October 23). Armour Thyroid Side Effects. Retrieved from https://www.healthline.com/health/armour-thyroid-side-effects#interactions
- Chandna, S., Bathla, M. Oral Manifestations of Thyroid Disorders and Its Management. Indian Journal of Endocrinology and Metabolism. 2011; 15(Suppl2): S113-116. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169868/
- General Information. (n.d.). American Thyroid Association. Retrieved from https://www.thyroid.org/media-main/press-room/