Pregnancy changes the whole body and the changes range from psychological-emotional swings to the more obvious physical changes. The mouth is not an exception to the many changes in the body.
Several conditions may appear during pregnancy, including pregnancy gingivitis, to even the beginning signs of postpartum depression.1 Poor oral health during pregnancy may lead to poor health for the mother and infant. Oral health should be considered as part of prenatal care.2
Hormones
Hormones can easily irritate the gingiva, increasing redness, tenderness, soreness, and bleeding. The hormonal imbalance during pregnancy heightens the response to irritation. A common condition is pregnancy gingivitis. For pregnancy gingivitis to happen, there needs to be a mixture of hormones, biofilm, and microbial flora.3
Estrogen and progesterone receptors are found in the periodontal tissues. The increase in these hormones during pregnancy affects the response of the tissues. An inflation in P.gingivalis, P.intermedia, and Tannerella have been found in subgingival plaque during the onset of pregnancy gingivitis. These bacteria are able to utilize the hormones, particularly progesterone, as nutrition.
With the boost in bacteria growth, hormones, and the use of the immune system sheltering in the gingival crevice, the bleeding gingiva provides further nutrients and the creation of a pocket depth, which all produces a more encouraging environment for anaerobes. In the microbial flora aspect gram-negative anaerobic bacteria are the main offenders in periodontal disease, while in pregnancy gingivitis, bleeding and inflammation have been associated with an increase in gram-negative rods.4
By the end of the third trimester, progesterone and estrogen have reached peak plasma levels. High levels of progesterone and estrogen can cause the ligaments and bone that support the teeth to loosen, resulting in the mobility of teeth. This usually subsides after pregnancy.2
Progesterone works as an immunosuppressant in the gingival tissues of pregnant women. Although this prevents a rapid acute inflammatory reaction against plaque, it allows an increased chronic tissue reaction, resulting in an exaggerated appearance of inflammation.2
Estrogen enhances vascular endothelial growth factor production in macrophages, which in turn is antagonized by androgens that may contribute to the development of a pregnancy tumor.3
During the pregnancy, the immune system is altered, including decreases in key players such as T-cell activity, neutrophils, antibody production, and lymphocyte responses. With those deficiencies, it is more challenging to control gingival issues.2
Pregnancy Gingivitis
With the increased reactive response to bacteria and plaque, pregnant women are more susceptible to periodontal disease. The most common condition is pregnancy gingivitis, affecting almost half of pregnant women. Pregnancy gingivitis commonly appears between the second and eighth months of pregnancy.2
Increased tooth mobility may happen even in the healthiest periodontium. This mobility is possibly due to mineral shifts in the lamina dura. The maxillary incisors are the most mobile during the last month of pregnancy and will resolve after birth.4
Having more frequent cleanings during pregnancy can help with calming the gingivitis. As it’s known, gingivitis, if not addressed, may become periodontitis and can promote preterm birth and low birthweight.2
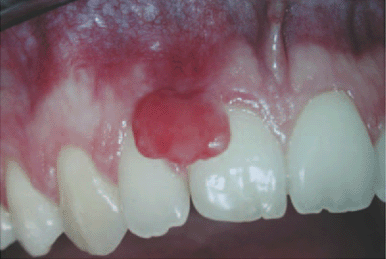
Pyogenic Granuloma
Pyogenic granuloma is a common tissue tumor, which affects up to 10% of pregnant women. It is an overgrowth of tissue due to irritation, trauma, or hormonal factors. This granuloma may be red, pink, or purple, growing rapidly. It may be smooth or mushroom-shaped and commonly seen on the labial surface of the papilla. Newer lesions appear red due to the abundance of blood vessels, and older lesions are pinker. During the first trimester up into the seventh month are when the lesions are most likely to occur.5
Pregnancy epulis is termed the “pregnancy tumor” since it occurs exclusively in pregnant women. The developed epulis (an enlargement on the gingival or alveolar mucosa) surfaces from hormonal changes and an increased inflammatory response to plaque or other irritants. This nonpainful, benign tumor is made up of capillary vessels and endothelial proliferation. It tends to bleed easily and appears red and inflamed.
The epulus appears mostly in the maxillary anterior region (see Figure 1). There is usually pregnancy gingivitis involved and commonly appears in the third trimester of pregnancy in up to 5% of pregnant women. After birth, it decreases or disappears.4,5
Morning Sickness
Unfortunately, morning sickness may become a common ritual. When vomiting occurs, stomach acid is a part of that mixture, and, when it reaches the mouth, it bathes the teeth. The increased acidity in the mouth encourages future erosive tooth wear. Regular morning sickness is an awful taste and thought. But waiting about 30 minutes to brush — although rinsing is fine — will prevent damage to the teeth.6
Gagging
Gagging can also be a new obstacle. Pregnancy may cause it or increase it. The nausea could cause neglect of the teeth. Gagging reflexes usually are triggered at the maxillary and the posterior teeth. The increase of vomiting, the challenge of gagging, more fatigue, and possible dietary changes all promote higher risk of decay.
Keeping up with home care is important during this time. Recommend a toothbrush with a smaller head or brushing at better times of the day when the gag reflex is weaker. To be able to do a decent cleaning, suggest brushing the mandible and anterior teeth first. At least that way, the majority of the mouth is cleaned before the gag reflex kicks in. Rinsing with water or mouthwash throughout the day may help with the extra challenges.
Diet
Eating healthy during pregnancy is important for the mother and baby, which includes the daily recommendations of vitamins A, C, and D, calcium, phosphorous, and proteins. The baby will leach calcium and vitamin D from the mother. If the mother doesn’t have enough calcium, the body will start to take it from the bones (not teeth).
The different cravings and an increased appetite could initiate a yearning for the carbohydrates and sweets that will increase the chance of decay.6
Taste Changes
A condition called dysgeusia leads to taste changes during pregnancy. The pregnant woman may prefer saltier and sweeter foods than when not pregnant. Some women may experience a metallic taste during pregnancy, which can aggravate nausea and suggest a nutrient imbalance. A metallic taste is common with the oestrogen hormone. The metallic taste may be annoying, but unfortunately, time and birth of the baby is the best cure. Other temporary solutions for relief are frequent brushing, interdental cleaning, and gargling with mint flavor products, consuming citrus foods, vinegar, sour foods, and sugarless gum.
The varying levels of oestrogen during pregnancy may also change the sense of taste throughout pregnancy.7 What tastes good one day may be nauseating the next day. During the first trimester, they may also experience a decrease in taste. Changes in taste may vary in each trimester. After birth, the mother may initially experience a dull taste but will improve to full capability.
TMD
The relaxin hormone helps soften the ligaments produced during pregnancy. This not only is to help make the pelvic area more elastic, but it also affects the jaw. Relaxin can make the jaw ligaments more elastic and unstable, allowing the mouth to open unpredictably wider than usual. When this happens, closing the mouth may need manipulation or assistance.8
A part of pregnancy is swelling due to the extra fluid and blood produced by the body. Swelling increases significantly at about 20 weeks and continues until birth. Some pregnant women may even experience fluid swelling in the face and neck that could promote pressure on the jaw and TMD.8
Gestational Diabetes
Gestational diabetes occurs in pregnant women who didn’t have diabetes prior to pregnancy. Hormonal and body changes, however, develop diabetes during pregnancy. Normally, glucose production increases in the pregnant mother with an increased amount of glucose transferring to the fetus promoting fetal growth and maintaining the mother’s nutritional status. Gestational diabetes happens when there’s insufficient production of insulin that stirs up the balance of friction between estrogen, progesterone, and insulin.
These changes interfere with the action of insulin as it binds to the insulin receptor in preventing glucose from entering the cells properly. Other risk factors are obesity or a family history of type 2 diabetes. Physicians will usually test for diabetes between 24 to 28 weeks.9
Blood sugar is more challenging to control while pregnant. Since poor sugar control correlates with periodontal disease, it can cause an overall oral health reaction, much like a match to gasoline.
Soon after delivery, gestational diabetes goes away. However, the chances of having diabetes type 2 increases after the pregnancy.9 If a pregnant woman has gestational diabetes, they may have more nausea with vomiting, strong cravings for sweet foods and drinks, and may experience extreme dry mouth. To aid in the relief of dry mouth, the patient can stay hydrated with drinking plenty of water or sucking on ice chips, or sugar-free lozenges, gum or candies throughout the day. Other ideas are to soothe or relieve dry mouth with gels and rinses that are intentionally for dry mouth.
Radiography
Although research has proven that radiographs are safe for pregnant patients, it’s still not fully accepted or wanted by individual patients. According to the ADA, “Studies of pregnant patients receiving dental care have affirmed the safety of dental treatment. The American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women reaffirmed its committee opinion in 2017: Patients often need reassurance that prevention, diagnosis, and treatment of oral conditions, including dental X-rays (with shielding of the abdomen and thyroid) … [is] safe during pregnancy.”10
On the other hand, “Some studies indicate that lead shielding is not necessary for dental radiographs for pregnant patients. A study published in 2016 measured the dose of radiation to the fetus and breasts with lead shielding and without lead shielding. The study found the dose with or without the lead shield was far below the level associated with harm to the fetus. The authors did add that this was technique specific.”16
Nitrous Oxide
Nitrous oxide is considered a Category C (risk cannot be ruled out) with the FDA classification system. Before use, a consultation with a physician is a good idea. The ADA recommends avoiding nitrous during pregnancy. If local anesthetic isn’t adequate, nitrous oxide may be used.10 Pregnant women require lower levels of nitrous oxide to achieve sedation.11
For a pregnant dental provider with regular exposure to nitrous oxide, it is less safe. Short, infrequent exposures are acceptable, but chronic exposure to nitrous oxide may cause harm to the fetus.
Nitrous oxide has been shown to oxidize vitamin B12 and impair synthesis of thiamine, folate, and thionine. It also increases short-term behavioral effects, decreased mental performance, audiovisual and manual dexterity, neurological effects, and renal and liver disease. In the worst cases, nitrous oxide could cause reduced fertility and spontaneous abortions.12
Dental Anesthetic
When local anesthetic is administered, it exposes both the woman and the fetus. Although dental anesthetic is safe in general, it’s recommended for after the second trimester. Lidocaine is the safest with almost no adverse effect on the mother or fetus. It is under a category B (no evidence of risk in humans) with the FDA classification system.
Also, keep mind if the pregnant woman has any medical complications that are pregnancy-related, they are more prone to experience side effects from the dental anesthetic.13 The severity of a local anesthetic side effect is based on the local anesthetic used, the amount, the method of administration, and the metabolic rate and half-life in the mother. The mothers who have hypertension or gestational diabetes may experience reduced blood flow to the fetus if epinephrine is used.
In women with eclampsia or preeclampsia, protein binding of local anesthetics is reduced. In effect, it will cause a large amount of local anesthetic to transfer to the fetus. Some medical complications considered are fetuses that are at high risk for asphyxia or poor general conditions.13
Dental Visit
The stage of pregnancy can dictate the comfort experienced during dental visits. Early in the pregnancy, morning sickness and nausea may be loathsome, and afternoon appointments may help. If it’s later in the pregnancy, lying supine in a dental chair may be uncomfortable.
The American Dental Association states,” Oral health care, including having dental radiographs taken and being given local anesthesia, is safe at any point during pregnancy. Further, the American Dental Association and the American Congress (formerly “College”) of Obstetricians and Gynecologists agree that emergency treatments, such as extractions, root canals or restorations can be safely performed during pregnancy and that delaying treatment may result in more complex problems.”10
Antepartum Depression
Antepartum or prenatal depression is depression during pregnancy, while postpartum depression is depression after pregnancy. During pregnancy, hormonal changes affect brain chemicals and could cause depression and anxiety. During depression while pregnant, a woman may have trouble caring for herself, placing her oral health on the back burner.14
Antepartum depression may lead to extra emotional and physical stress. This increases miscarriages, preterm births, and low birthweight.14
With additional health risks and conditions with pregnancy, it is best to encourage meticulous home care. If periodontal disease, diabetes, depression, or lack of home care is involved, extra attention with a professional prophy along with at-home cleaning should be stressed. Some insurance plans will cover an extra prophy during pregnancy. But even if they don’t, it may still be a good idea to encourage the benefit of one.
Need CE? Click Here to Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Postpartum Depression. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617.
- Pregnancy and Oral Health. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/oralhealth/publications/features/pregnancy-and-oral-health.html.
- Gondivkar, S.M., Gadbail, A., Chole, R. Oral Pregnancy Tumor. Contemp Clin Dent. 2010; 1(3): 190‐192. Retrieved from http://www.contempclindent.org/article.asp?issn=0976-237X;year=2010;volume=1;issue=3;spage=190;epage=192;aulast=Gondivkar.
- Pirie, M., Cooke, I., Linden, G., Irwin, C. Dental Manifestations of Pregnancy. Obstetrics & Gynecology. 2007; 9(1). Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1576/toag.9.1.021.27292.
- Rabinerson, D., Kaplan, B., Dicker, D., Dekel, A. (2002) Epilus During Pregnancy. National Library of Medicine. 2002 Sep; 141(9): 824-6, 856-857. Retrieved from https://pubmed.ncbi.nlm.nih.gov/12362490/.
- Healthy Mouth. Pregnant? 9 Questions You May Have About Your Dental Health. American Dental Association. Retrieved from https://www.mouthhealthy.org/en/pregnancy-slideshow.
- Metallic Taste During Early Stages of Pregnancy. Retrieved from https://www.huggies.com.sg/en-sg/parenting-center/pregnancy/metallic-taste-during-early-stages-pregnancy.
- Bayramova, A. TMD and Pregnancy? Clin J Obstet Gynecol. 2018; 1: 001-006. doi: 10.29328/journal.cjog.1001001.
- Gestational Diabetes and Pregnancy. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/pregnancy/diabetes-gestational.html.
- Oral Health Topics. Pregnancy. Key Points. American Dental Association. August 13, 2019. Retrieved from https://www.ada.org/en/member-center/oral-health-topics/pregnancy.
- Oral Health Care During Pregnancy Expert Workgroup. 2012. Oral Health Care During Pregnancy: A National Consensus Statement. Washington, DC: National Maternal and Child Oral Health Resource Center. Retrieved from https://www.mchoralhealth.org/PDFs/OralHealthPregnancyConsensus.pdf.
- Olfert, S. Reproductive Outcomes Among Dental Personnel: A Review of Selected Exposures. Professional Issues. J Can Dent Assoc. 2006; 72(9): 821-5. Retrieved from http://www.cda-adc.ca/jcda/vol-72/issue-9/821.pdf.
- Lee, J.M., Shin, T.J. Use of Local Anesthetics for Dental Treatment during Pregnancy, Safety for Parturient. J Dent Anesth Pain Med. 2017; 17(2): 81–90. doi:10.17245/jdapm.2017.17.2.81. Retrieved from https://www.researchgate.net/publication/318366249_Use_of_local_anesthetics_for_dental_treatment_during_pregnancy_safety_for_parturient
- Depression During Pregnancy & Postpartum. Postpartum Support International. Retrieved from https://www.postpartum.net/learn-more/depression-during-pregnancy-postpartum/.
- Depression in Pregnant Women and Mothers: How It Affects You and Your Child. Caring for Kids. March 2017. Retrieved from https://www.caringforkids.cps.ca/handouts/depression_in_pregnant_women_and_mothers.
- Hatfield, S. Radiology Update: Evolving Standards for Pregnancy, Shielding, and Frequency. Today’s RDH. March 14, 2020. Retrieved from https://www.todaysrdh.com/radiology-update-evolving-standards-for-pregnancy-shielding-and-frequency/