It’s 2018, and to my surprise, there are many dental practices still using film radiographs. Although there is nothing wrong with film radiographs, we can all attest that digital images offer not only lower exposure to radiation but also clearer images versus traditional film. With clearer images, the doctor can make an accurate diagnosis in the treatment planning, and you as the hygienists, can provide the best recommendations to the patient, right? As a hygienist, I did believe my patients were receiving the best recommendations we had to offer until the cone beam computed tomography scan, or CBCTs/CT scan, caused a paradigm shift in how I now approach my patients’ oral health care.
Let’s think about this, I mean really think about this for a moment.
How many times have you seen an emergency toothache patient added to your office’s schedule? What if your patient says the tooth with the “watch” on it has not settled or they’re having pain in their gums, what do you do? If your patient has a history of sinus problems and they’re having pain in their upper posterior area, what is your recommendation? The standard protocol includes taking an image of the tooth in question, perhaps measure the pocket depths around the tooth, and wait for the doctor to diagnose. If the doctor diagnoses the image to be within normal limits, the recommendations we often state varies from: when the sinus issues resolve, the pain should resolve. Or you may have bit down hard on something, try to eat on the other side for a couple of days. Or even you may be clenching during your sleep; maybe a night guard will help. Do any of these recommendations sound familiar to you? Currently, this protocol is not negligence, but, what if it is?
I came across a patient who was experiencing gingival pain in the lower right quadrant. Tooth number 31 was endodontically treated. A 2D digital image was taken, and the doctor found no obvious concerns. The patient was referred to the dental imaging center where I am employed, and we did a 3D cone beam CT scan. The CT results showed bone loss on the mesial wall and through the furcation of tooth number 31.
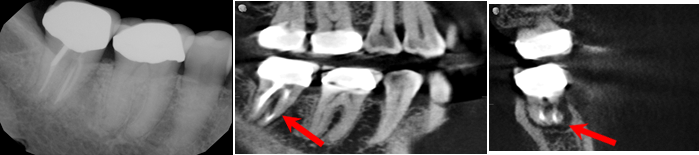
I also came across multiple referred patients with a history of sinus problems, who presented to our imaging center experiencing a toothache, and the 2D digital image that was taken at their dental home showed no obvious concerns. The 3D cone beam CT scan we took showed a defect in the bone and the infection draining into the sinus like the example pictured here.
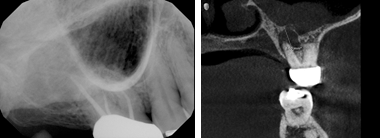
Seeing the results of their images made me wonder; is the patient’s sinus infection caused by a nasal infection or a tooth infection draining into the sinus cavity? When a patient presents with a chief complaint regarding their gingiva, I assume a popcorn kernel could be lodged subgingivally or perhaps flossing trauma. Now I’m wondering, could the pain be bone loss occurring that is not yet viewable on a 2D digital image? What about our patients who present to their appointment with no chief complaints and their periodontal assessments and 2D digital images appear fine? Are those patients really within normal limits with no obvious concerns?
These questions I began asking myself created an “ah-ha light bulb” moment for me and WOW, was I excited! I was excited to ask the doctors that do not currently refer out or use a 3D cone beam CT scan on their patients these questions, and I look forward to challenging their thought process. If specialty practices such as Endodontist and Oral Surgeons utilize the 3D cone beam CT for their patients’ treatment planning, why aren’t the General Practitioners considering the use of 3D cone beam CTs for their patients? Whether it’s referring their patients out to an imaging center or purchasing their own, a 3D cone beam CT scan implemented into the practice as the new standard of care benefits the patient and the practice. It creates a true preventative approach for the practice by identifying areas that may need to be addressed before the patient experiences any symptoms. There may be problematic areas other than what is currently treatment planned, or there may be no significant findings and the patient is truly within normal limits.
A cone beam CT scan is not only used to rule out pain of unknown origin or pathology but can also assess their airway for areas of possible airway obstruction. Your patients will leave their appointment appreciating and knowing they are receiving a thorough examination. So, how accurate are diagnoses based off film radiographs or 2D digital images?