Some hygienists would like autonomy working separately from the traditional dental practice and without the restrictions of a governing body, dentists, who have control of our clinical careers. We may feel limited in what we can say, the use of our skills, or our value as dental hygienists are not completely tapped into.
Are we missing the opportunities to elevate not only our individual dental hygiene careers but also the industry?
Hygienists may like to independently make treatment choices based upon not only current research but their experience in what they find has worked and what hasn’t worked. The goal always is to assist the patient’s health and well-being.
I personally would like some liberty as to where I practice and how to use my knowledge of not only dentistry but oral-systemic relationships. Wouldn’t it be grand to be a liaison between dentistry and other health care specialties, which may include involvement with cardiologists, gerontologists, or endocrinologists? Employment opportunities within a hospital or clinic shouldn’t be so far and few between. Do I need to become a licensed practical nurse or medical assistant to look inside a patient’s mouth in a physician’s office?
I personally would like collaborative involvement with other disciplines to utilize my expertise with dementia prevention as related to oral health. It isn’t just about an independent practice per se but to somehow use our knowledge, experience, and skills to help the health of all people. How about being included with the rest of health care?
Deciding on Role with Medicine
A question that comes up often is how do we exactly reach the other health care communities? Do we want to integrate into all of health care or to be collaborators? It may seem like just semantics, but it really isn’t.
Twenty years ago, the Office of the Surgeon General published the first report on oral health.1 The purpose was to alert Americans that oral health had significant importance to general health and well-being. Oral systemic health is the phrase that dentistry talks about, and the public is starting to understand.
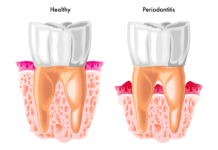
“Yes, Virginia, the mouth and body are intricately connected.” The human body is made up of multiple systems that work together to form life. Body systems are an organized group of tissue that form a particular function. These functions work with other systems in the body. The main systems of the body are digestive, circulatory, nervous, respiratory, and muscular. Not one of these does not need each other to function, and the building block of all living things are cells ─ trillions of cells. It was designed together to work together.
In the same vein, all health disciplines should work together to keep the trillions of cells working harmoniously. We, the collective cells, are the ones who are not working together. Dental education creates good clinicians but is limited in the perspective of overall health. Medicine is similar; good clinicians but limited education about oral health. A separation between the disciplines has a rich history that is proving hard to change. Our offices are separate, our pay system is different, and finding the time to consult with another specialty is an insurmountable task.
In recent years, there have been gains such as Kaiser Permanente Northwest in Oregon that has a truly integrated medical-dental practice. It isn’t necessarily one group disagreeing more than another for unification, but there is pushback from our own community. The reasons range from no buy-in about oral-systemic health to no desire to join the health insurance world, as well as how the melding of medical records is a hiccup.
Dentists like autonomy. Questions arise if we want to truly integrate or collaborate. What is the difference?
Integration
There are many definitions of integration and opinions about those definitions. Some incorporate “the combining into a complete and harmonious whole.” Integration inside health care is often referred to as interprofessional health care and does have a high degree of collaboration and communication between health professionals, but dentistry is most often not included.
The uniqueness of health integration is not only sharing information related to biologics but the psychological and social needs of a patient. The providers will collaborate and design a comprehensive treatment plan. Integrated care, as defined in Wikipedia, speaks of coordinated care or seamless care. (Really? Health care that is seamless?) It brings together the delivery and management of services, and dentistry clearly is not in the “system.”
To integrate, we must use the same billing system, language, and metrics. Pacific Dental Services, a dental support organization (DSO), joined Epic System’s electronic health record (EHR) system, for example, to improve care coordination ─ no small feat, to put it mildly. Time, energy, training, and the financial undertaking were enormous. The United States Department of Veterans Affairs is the largest integrated care delivery system in the United States. Among private systems, according to 2019 data, is HCA Healthcare with 185 hospitals and Ascension with 151.
A few dental practices are a part of large health care organizations, including Kaiser Permanente’s Health Partners and federally qualified health centers (FQHC) where dentists and physicians can work side by side helping patients.2
The current integrative system in traditional health care is not without problems. The struggle with communication, coordination, and referral is ongoing. A primary care physician potentially has to coordinate with a large number of physician colleagues daily for many of their patients. One study showed that for 100 Medicare patients, the average primary care practitioner needed to coordinate with 99 other physicians working in 53 practices.4
In July 2021, an extensive review was published looking at integrated care of patient-centered medical homes. To have success with comprehensive primary care, there are extensive barriers even though we know how much it would benefit patients.3
A term used often when talking about integrations is “silo.” A siloed dental profession can’t solve a patient’s oral health problems alone. The medical profession can’t solve the general health problems alone. Integration implies fusion, unification, combining, and merging. By contrast, collaboration involves organizing distinct entities to function together efficiently and effectively. Collaboration and coordination can be achieved without integration, but integration without internal interdisciplinary collaboration and coordination doesn’t necessarily achieve the ultimate purpose. Therefore, bridging the health care silos to achieve interdisciplinary collaboration and coordination is foundational, regardless of whether it evolves into fully integrated healthcare systems.
In 2019, The American Academy of Oral Systemic Health hosted its annual conference titled Collaboration Cures. I never thought longer than a second about the title that I am sure others painstakingly created. The American Academy of Physiological Medicine and Dentistry’s fifth annual meeting had the same title; Collaboration Cures Airway Summit.
Collaboration is defined as working jointly together, perhaps for a common goal ─ better health, I would say. Integration is really a single organizational framework vs. collaborating is working closely together. Of course, when integration has occurred, collaboration will happen. Maybe not seamlessly, but it will occur. We need more interprofessional collaboration first, not necessarily to join into a system that may take decades to be fully entrenched. We need change now, and the beginning step is to collaborate.
Collaboration
I became acquainted with a dentist from Colorado, Dr. Larry Coffee. Dr. Coffee was the founder of Dental Lifeline Network (DLN) that established Donated Dental Services. Within two years, the organization turned into a national humanitarian resource for needy, disabled, elderly, and medically compromised people. His eloquence of speech is like no one I have ever encountered, and I am humbled every time we connect. His kindness pours out of him and ends all emails “in friendship,” which I think he means.
We were in deep discussion about a webinar I was involved in, and he said, “Oral health literacy is terribly inadequate ─ not just among at-risk populations, but also the health care and social work providers on which many depend.” We spoke about trying to “bridge the health care silos” and how to start small, such as throwing a pebble in the pond that generates ripples as opposed to huge boulders that create waves.
There is resistance in the joining or the coalition of forces to a degree, but Dr. Coffee shared with me a document, “Clinical Consensus of Medically Necessary Dental Care.” The document included 20 medical associations, including The American College of Cardiology and the American Diabetes Association.
All of these medical associations shared their professional perspective about the importance and relevance of oral and dental health to the management and treatment of diseases within their respective disciplines. Many specified specific diseases, conditions, and procedures where the resolution of oral and dental infections was imperative. Some included rheumatoid arthritis, Parkinson’s, congestive heart failure, diabetes mellitus, AIDS, hepatitis, lupus, osteomyelitis, cancer, ALS, and multiple sclerosis. It was an agreement. Period. Them (medicine) and us (dentistry) agreeing.
“Start low, go slow” is a truth in pharmacotherapy for many diseases that also offers practical guidance when trying to build a coalition of groups with different backgrounds, interests, and priorities. Ease into the process by minimizing issues that may be controversial, such as a domination of one profession over another. Keep in mind obstacles such as a bad history, turf issues, or my way is the only way attitude before adding even more complexities as the relationship matures.
Ultimately, the purpose of advancing meaningful interdisciplinary relationships among health care professionals is to support the health and well-being of people, individually and collectively. That is the most ambitious goal. The strategic means for achieving it will undoubtedly be an evolutionary process requiring the resolution of many obstacles, including professional resistance, liability concerns, scope of practice regulations, distinct academic programs, insufficient supportive data, and lack of insurance coverage.
Perceptions can also become a major snag, obstructing and complicating change thought to be threatening, complex, and costly. Because the terminology used to describe intentions can affect perceptions, it may be more disarming and unsettling to refer to medical/dental/behavioral health/pharmacy collaboration rather than integration as the means for advancing patient-focused care.
Dr. Coffee posed something interesting in our discussion. “On the topic of perception influencing the meaning of terminology, the phrase oral/systemic health may elicit a somewhat narrow meaning of oral health as it relates to medical status. If that is the intent, it works. Yet, the bi-directional impact of oral health and total well-being is broader, encompassing psychological and social circumstances as well. I would value your thoughts about the following alternative: Dental health ↔ overall health and well-being.” Something to think about, isn’t it?
Collaboration in health care can be defined as professionals assuming complementary roles and cooperatively working together, sharing responsibilities for problem-solving, and making decisions to form and carry out plans for patient care.5,6
How Do We Collaborate?
Collaboration brings different members with unique skill sets together to provide exceptional care for patients. Unfortunately, as dental hygienists, our collaboration with other health professionals requires most often supervision by a dentist, reducing any authority in the equation. Even though collaboration is interdependent, having autonomy is important. The main goal always is to do the right thing with your patient in mind.
The physical proximity of dental practices to other health care professions is unlikely to be mainstream for many years. The consultation and referral process may become more streamlined by increasing the communication among providers and between providers and patients. Telemedicine and teledentistry have probably helped a bit. Collaboration between professionals is also difficult because of the poor understanding of one another’s practices. Even across members of the same discipline, communication and referral to other providers can be challenging, but we still must try to put unique systems in place that will work for us and the practice you work for.
Too often, we have broad ideas with no actionable steps for immediate or future implementation. I am all about planning, but what can we do right now? The immediate implementation must occur now, and many of you are doing it. You are talking to anyone in health care who will listen about the importance of oral health to whole-body wellness.
For those of us who are not, remember it doesn’t need to be a formalized lecture or article. No dissertations needed. Talk with your patient about their heart, their medications, and anything you see that may need cooperation from a medical provider to start the dialogue. Learn about providers in your area who would be willing to talk to you with collaboration in mind. Speak with your own doctor, your family member who may be a nurse, your chiropractor. Blaze a trail. Opportunities abound.
Many of us in dentistry know this, but let’s always remember the quote from Dr. C. Everett Koop, the former Surgeon General: “You’re not healthy without good oral health.”
Need CE? Click Here to Check Out the Self-Study CE Courses from Today’s RDH!
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Oral Health in America: A Report of the Surgeon General. (2000). National Institutes of Health, National Institute of Dental and Craniofacial Research, U.S. Department of Health and Human Services. Retrieved from https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf
- Jones, J.A., Snyder, J.J., Gesko, D.S., Helgeson, M.J. Integrated Medical-dental Delivery Systems: Models in a Changing Environment and Their Implications for Dental Education. Journal of Dental Education. 2017; 81(9): eS21–eS29. Retrieved from https://doi.org/10.21815/JDE.017.029
- Gupta, A., Akiya, K., Glickman, R., Silver, D., Pagán, J.A. (2021). How Patient-centered Medical Homes Integrate Dental Services into Primary Care: A Scoping Review. Medical Care Research and Review. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34238063/
- Pham, H.H., O’Malley, A.S., Bach, P.B., Saiontz-Martinez, C., Schrag, D. Primary Care Physicians’ Links to other Physicians through Medicare Patients: The Scope of Care Coordination. Annals of Internal Medicine. 2009; 150(4): 236–242. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19221375/
- Fagin C.M. Collaboration between Nurses and Physicians: No Longer a Choice. Academic Medicine: Journal of the Association of American Medical Colleges. 1992; 67(5): 295–303. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1575859/
- Baggs, J.G., Schmitt, M.H. Collaboration between Nurses and Physicians. Image–the Journal of Nursing Scholarship. 1988; 20(3): 145–149. Retrieved from https://sigmapubs.onlinelibrary.wiley.com/doi/10.1111/j.1547-5069.1988.tb00055.x