Oral cancer awareness is something that, as hygienists, should always be at the forefront of our practice. April is Oral Cancer Awareness Month, which is a good time to hone our skills and encourage one another in our knowledge of oral cavity and oropharyngeal cancer and the importance of screening all our patients.
Oral cavity and oropharyngeal cancers fall cancer falls under the umbrella of head and neck cancers. These types of cancers are the sixth most diagnosed in the entire world.1
The American Cancer Society estimates there will be about 58,450 new cases of oral cavity or oropharyngeal cancer in the United States in 2024. In men, these cancers are twice as common as in women, with the mean age of diagnosis being 64.2 However, this is changing rapidly, and younger people are being diagnosed, partly due to the human papillomavirus (HPV).1,2
Early Detection Remains Key
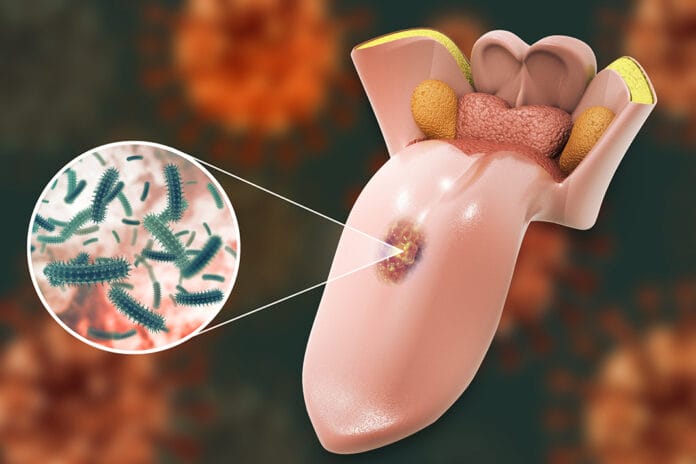
Malignancies can occur anywhere, but common sites for oral cavity malignancies include those of the tongue and the floor of the mouth. The buccal mucosa and gingiva are common sites for those who use chewing tobacco. The base of the tongue, soft palate, pharyngeal wall, tonsillar crypts, and tonsils are common sites for oropharyngeal malignancies, especially in younger people who don’t smoke.3
Sadly, oral cavity and oropharyngeal cancers continue to have a poor prognosis. If diagnosed early, within stage I or II, the five-year survival rate can can exceed 80%. Unfortunately, nearly half of all oral cancers are not diagnosed until later, within stages III and IV.4 The five-year survival rate for later-stage cancers of the tongue, the floor of the mouth, lip, and oropharynx areas can decrease between 23% and 41%, depending upon the location.5
Our patients often spend more time with us during a recare appointment than the doctor, which makes dental hygienists the clinicians who detect these cancers.
Risk Factors
We know many aspects of a dental hygiene appointment are extensive, so adding anything else to appointments can feel overwhelming. One idea to streamline discussing oral cavity and oropharyngeal cancers with our patients would be to add certain questions to the medical history form that specifically address known risk factors.
Examples of risk factors include tobacco use and alcohol consumption. A simple yes or no could suffice. More in-depth questions could be asked about how many drinks are consumed per day/week and how much tobacco is used per day/week. Further examples include betel nut and quid chewing history, HPV diagnosis, and if the patient has received an HPV vaccine.
Tobacco ‒ Tobacco use of all kinds increases the risk of oral cancer. This includes cigarettes, cigars, pipes, and smokeless tobacco. There is a positive correlation between the amount of tobacco use and the likelihood of developing oral cancer.3,4,6
Alcohol ‒ Alcohol use is also linked to an increased risk of oral cancer. Similarly to tobacco use, the more a person consumes alcohol, the higher their chances of developing an oral malignancy.3,4,6
According to the American Cancer Society, the risk of developing oral cancer increases 30 times when consuming both tobacco and alcohol compared to their counterparts who consume neither.6
Betel quid ‒ Betel quid, also known as gutka, is a mixture of betel nut, tobacco, and other cancer-causing ingredients. It is used throughout Asia and may be seen in specific patient populations. It is typically used like traditional smokeless tobacco, placed into the cheek, and kept for long periods.4,6,7
Human papillomavirus ‒ HPV includes a group of over 200 different viruses. Out of these 200 strains, around 12 are considered high risk for their potential to cause cancer. To date, research shows that two of these high-risk strains, HPV 16 and HPV 18, account for most HPV-related cancers. Since HPV infects squamous cells, HPV-related cancers are considered squamous cell carcinomas.8
While we know HPV can cause cancer in numerous areas of the body, hygienists should be concerned about the risk of HPV-related cancer, specifically because of our area of expertise. The area most at risk for HPV-related cancer is the oropharynx. About 70% of oropharyngeal cancers are caused by HPV.8
An HPV vaccine has been administered since 2006 and is estimated to reduce the risk of developing HPV-related cancers by more than 90% when administered to kids between the ages of nine and 12. In addition to protecting against the two strains of HPV that are responsible for genital warts, the vaccine also protects against seven other strains that may lead to HPV-related cancers.8,9
Screening and Diagnosis
Hygienists should be encouraged to use any screening and adjunct tools they have available to them. The use of loupes and a headlamp can be crucial to the early detection of potentially malignant lesions.
No matter the adjunct tools used, it is imperative to utilize intraoral photography and document a detailed description of the lesion in the patient’s chart, such as location, distribution, margins, size and shape, color, consistency, surface texture, and lesion history. This is important so that any clinician who may see the patient can have a point of reference, and it can also be helpful when referring a patient to another specialist.
If a lesion persists for two weeks or more once all possible irritants, such as sharp teeth, restorations, and appliances, have been removed, the gold standard continues to be a biopsy.4 “The presence or absence of dysplasia is not directly associated with a specific clinical appearance of the lesion, so it is not possible to predict whether dysplastic alterations are present before performing biopsy.”4
Referral
If your dental practice does not perform its own biopsy services, it is imperative to have a good relationship with your local periodontists, oral surgeons, oral pathologists, and ear, nose, and throat doctors (ENTs). The responsibility of cultivating these relationships often falls to the doctor, but hygienists can also advocate for this close working relationship to provide the best care to our patients. A referral to an ENT may be warranted for lesions in the tonsillar and posterior oropharyngeal area.
To make it convenient and easy to access, hygienists may want to keep all referral slips in one place and organize them by specialty (i.e., oral pathologist, ENT). Referral slips can be kept in the operatory or at the front desk.
To eliminate miscommunication, there should be an office protocol on who will fill out the referral slips and follow up with the patients to see if they’ve scheduled the recommended appointment. As we know, documentation is key, so it may be good practice to have the front desk scan a copy of the referral slip into the patient’s chart and document in the chart that a referral was given.
Even if your office isn’t the one receiving the original pathology report, it is always a good idea to request a copy to keep in the patient’s chart. Beyond having a copy for record-keeping purposes, this can also be helpful for patient care and education. For example, if the pathology report gives specific information on what the patient can do to prevent a recurrence of a type of lesion, such as avoiding spicy foods or mint oral hygiene products, we can reinforce this at subsequent hygiene visits and offer alternatives for products when needed.
What We Can Help Our Patients Do
We can show patients the areas in their mouth that are most at risk for developing oral cancers and encourage self-exams. We know that what our patients do at home after they leave our chairs is imperative to their overall health.
As hygienists, we are constantly tailoring our recommendations to our patients. Being aware of patients’ lifestyle risks can be extremely helpful for educating our patients on their risk of developing oral cancer.
Performing oral cancer screenings on every patient, every time, taking photos as needed, recommending a two-week follow-up for suspicious lesions, and referring our patients to other trained specialists when necessary are all ways we can keep our patients healthy.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Rodríguez-Molinero, J., Migueláñez-Medrán, B.D.C., Puente-Gutiérrez, C., et al. Association Between Oral Cancer and Diet: An Update. Nutrients. 2021; 13(4): 1299. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8071138/
- The American Society Medical and Editorial Team. (2024, January 19). Key Statistics for Oral Cavity and Oropharyngeal Cancers. American Cancer Society. https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html
- Oral Cancer Facts. (n.d.). Oral Cancer Foundation. https://oralcancerfoundation.org/facts/
- Abati, S., Bondi, S., Bramati, C., et al. Oral Cancer and Precancer: A Narrative Review on the Relevance of Early Diagnosis. Int J Environ Res Public Health. 2020; 17(24): 9160 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7764090/
- The American Cancer Society Medical and Editorial Content Team. (2023, March 1). Survival Rates for Oral Cavity and Oropharyngeal Cancer. American Cancer Society. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/detection-diagnosis-staging/survival-rates.html
- The American Society Medical and Editorial Team. (2021, March 23). American Cancer Society. https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/risk-factors.html
- Betel Quid with Tobacco. (n.d.). NIH: National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/betel-quid-with-tobacco
- HPV and Cancer. (2023, April 4). NIH: National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
- The American Cancer Society Medical and Editorial Content Team. (2020, August 4). HPV Vaccine Facts. American Cancer Society. https://www.cancer.org/healthy/cancer-causes/infectious-agents/hpv/hpv-vaccine-facts-and-fears.html