Sleep-related breathing disorders are becoming more well-understood by the medical and dental communities. Sleep apnea, one of multiple sleep-related breathing disorders, has been implicated as a risk factor for numerous systemic chronic diseases. Sleep apnea affects millions of Americans each year. An estimated 2-9% of the American population has one type of sleep apnea.1
With emerging research and continuing education opportunities, dental professionals are recognizing how they can help patients become aware of clinical signs and symptoms of sleep apnea and recommend follow-up evaluations with their primary care physician or a sleep medicine specialist. Dental professionals are in the perfect position to screen patients as many signs and symptoms can be observed through oral clinical exams.
Clinical Indications
Clinical signs that can increase the risk of sleep apnea include a high-arched or narrow hard palate, redness of the soft palate and uvula area, limited tongue space/macroglossia, micrognathia, retrognathia, nasal septum deviation, and adenotonsillar hypertrophy.2,3 Adenotonisllar hypertrophy (i.e., enlarged adenoids and tonsils) is the most common risk factor for sleep apnea in children.2
Along with clinical signs, patients may experience symptoms such as daytime sleepiness, headaches, bruxism, and a constant feeling of unrest despite sleeping the recommended seven to nine hours a night. Patients who report these symptoms and display signs of airway obstruction would likely benefit from a sleep study.1,4
Diagnosing Sleep Disorders
Interprofessional collaboration is an intricate part of addressing sleep-related breathing disorders. Patients can discuss their options with their primary care physician, but a better route may be to refer the patient directly to a sleep medicine specialist for evaluation.1
Sleep studies can help diagnose multiple sleep-related breathing disorders, including sleep apnea, sleep-related seizure disorders, sleep-related movement disorders, as well as narcolepsy. Any of these disorders can contribute to daytime sleepiness and an overall feeling of fatigue. Determining the cause of the symptoms is essential for determining the proper treatment route.5
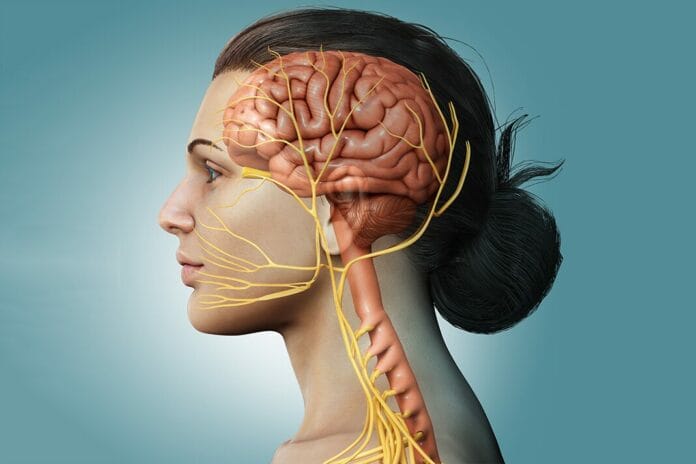
If the patient is diagnosed with sleep apnea, it could be classified as obstructive, central, or mixed. Obstructive sleep apnea is caused by the physical blocking off of the airway, whereas central sleep apnea involves a miscommunication between the brain and the muscles that control breathing, which stops a person from breathing while they sleep. Mixed sleep apnea is a combination of obstructive and central sleep apneas.1
Treatment with Hypoglossal Nerve Stimulation
Patients diagnosed with sleep hypopnea or mild sleep apnea have choices for treatment options, including continuous positive airway pressure (CPAP), oral appliance therapy (OAT), and/or behavioral modifications (weight loss, positional therapy). Historically, patients diagnosed with moderate to severe sleep apnea have been limited to CPAP and surgery.4
A newer treatment called hypoglossal nerve stimulation is now another option for patients diagnosed with moderate to severe obstructive sleep apnea. In 2014, the Food and Drug Administration (FDA) approved the Inspire upper airway stimulation system for patients 22 years and older, where a wire is surgically implanted in a patient’s body which stimulates the hypoglossal nerve through the power of a wire, remote control, and app on a patient’s cellular device.1,6 In 2020, the FDA expanded its approval for patients who met eligibility requirements to those 18 years of age and older.1
The hypoglossal nerve is the 12th cranial nerve that affects the tongue. The hypoglossal nerve controls the ability to swallow, speak, move the tongue freely, and make noises other than speech.7 The nerve can be found on the tongue’s lateral borders and ventral surface.7 This motor nerve plays a considerable role in many cases of obstructive sleep apnea because obstructive sleep apnea is often caused by the tongue blocking off the airway, as mentioned above.2
To be an ideal candidate, a patient must meet specific requirements, such as an obstructive sleep apnea diagnosis, BMI under 32, no concentric collapse of the soft palate, and have tried but been unsuccessful in accepting or adhering to CPAP.1,6
Hypoglossal Nerve Stimulation Procedure
During an outpatient procedure, an Inspire-certified sleep medicine specialist places a small impulse generator beneath the clavicle, a tunneled breathing sensing lead between the external and intercostal muscles, and a tunneled stimulation lead attached to the hypoglossal nerve branch that produces tongue protrusion during sleep.1,6
Recovery after surgery is typically a few days, with the patient being able to resume strenuous activities after two to four weeks. Pain, in most cases, can be managed with over-the-counter pain medication.1,8
About a month after surgery, the patient returns for a follow-up appointment to activate the device and learn how to use it. Once activated, the patient slowly increases the amount of stimulation to best meet their needs. After this “step-up process,” a follow-up sleep study is performed to ensure the device is meeting treatment goals.6,8,9
A patient should have their device checked by their sleep medicine specialist once or twice per year.6,8,9 The battery has a lifespan of approximately 10-12 years. At that time, another outpatient procedure is necessary to replace it.1,8
Patient Precautions
It is recommended that patients notify their physicians and dental providers that they have an implanted stimulation system and carry their Inspire Medical Systems ID card at all times.9
The Inspire system implant manual states that the implant pulse generator (IPG) “is designed to ensure immunity from most common sources of electromagnetic disturbance. In most cases, turning off the electromagnetic disturbance source or moving away from the electromagnetic disturbance source will return the IPG to normal operation.”9 Patients are recommended to use the therapy only while asleep to reduce the possibility of electromagnetic interference.9
The manual also states that “extremely strong sources of electromagnetic disturbance could interfere with normal IPG operation, causing the IPG to reset and requiring the IPG to be reconfigured.”9 Strong sources include defibrillation with an AED, radiation therapy for cancer treatment, and MRIs on their chest or torso.9 Therefore, patients requiring frequent chest or torso MRIs for specific medical conditions must discuss this with their sleep medicine physician before placement.1
According to the manual, diagnostic radiographs, such as dental radiographs, should not affect the Inspire system.9 If a dental professional has any concerns about the treatment of a patient with the Inspire system, reaching out to the patient’s sleep medicine specialist is recommended.
The Dental Professional’s Role
Dental professionals can help guide and educate their patients who present with signs and symptoms of sleep-related breathing disorders. Good chairside education can help to enlighten dental patients about how sleep-disordered breathing and sleep apnea can cause damage to teeth and oral tissues and potentially lead to various systemic health conditions.2
In addition to a medical history review and assessing signs and symptoms, simple clinical indices and short questionnaires such as the Mallampati score or STOP-Bang can help determine a patient’s risk for obstructive sleep apnea.2,4 The STOP-Bang questionnaire includes questions dental professionals can ask patients related to symptoms such as snoring, tiredness, and observed pauses in breathing during sleep.2
A dental professional should refer and encourage patients to be further evaluated by a sleep medicine specialist if necessary. Interprofessional collaboration is key to ensuring patients receive comprehensive care.2
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Foutain, L. (2023, November 3). What Is Inspire Sleep Apnea Treatment and How Does It Work? Sleep Foundation. https://www.sleepfoundation.org/sleep-apnea/what-is-inspire-sleep-apnea-treatment
- Gianoni-Capenakas S., Gomes, A.C., Mayoral, P., et al. Sleep Disorder Breathing: The Dentists’ Role – A Systemic Review. Journal of Dental Sleep Medicine. 2020; 7(1). http://dx.doi.org/10.15331/jdsm.7108
- Slowik, J.M., Sankari, A., Collen, J.F. Obstructive Sleep Apnea. (2022, December 11). StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK459252/
- Berggren, K., Broström, A., Firestone, A., et al. Oral Health Problems Linked to Obstructive Sleep Apnea Are Not Always Recognized within Dental Care – As Described by Dental Professionals. Clinical and Experimental Dental Research. 2022; 8(1): 84-95. https://doi.org/10.1002/cre2.517
- Sleep Studies. (2022, March 24). NIH: National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/sleep-studies
- The Emerging Option of Upper Airway Stimulation Therapy. (2018, February 10). Mayo Clinic. https://www.mayoclinic.org/medical-professionals/pulmonary-medicine/news/the-emerging-option-of-upper-airway-stimulation-therapy/mac-20431242
- Hypoglossal Nerve. (2021, June 4). Cleveland Clinic. https://my.clevelandclinic.org/health/body/21592-hypoglossal-nerve
- Chio, E. 2023. Upper Airway Stimulation. The Ohio State University. https://wexnermedical.osu.edu/ear-nose-throat/sleep-surgery/upper-airway-stimulation
- Inspire System Implant Manual [200-079-101 Rev A_5]. (2014). Inspire Medical Systems. https://www.accessdata.fda.gov/cdrh_docs/pdf13/P130008d.pdf