At my current office, I am probably considered a health history nag, but I am okay with that! I would prefer to be known for this because patients are then actively involved in their dental care when they participate in updating their health history at EVERY appointment. When hygienists involve patients this way, we are able to educate patients on how their whole health can contribute to dental diagnoses. With the knowledge of medications and new and previous medical diagnoses (i.e., Sjogren’s, cancer, diabetes), we are better able to connect the dots on the how and the why of various dental conditions that patients present with. In turn, this becomes a roadmap to our appointments. Making health history updates a priority is a must; there are no excuses for not taking a few minutes to do this for patients and ourselves. Mainstreaming this process can be made quite simple with patients chairside.
How often should we update our health histories, you ask?
While attending the Rocky Mountain Dental Convention (RMDC) recently, I attended the most informative class of my career, when it comes to an understanding what we, legally, should be considering. The dentists and lawyers (Dr. Robert Anderton, Dr. Mitchell Gardiner, Ms. Joy Jagol, and Mr. Ryan Donihue) leading the class were adamant that medical histories should be reviewed every time we see a patient. This is because we never know what can happen in a 24, 48, or 72-hour period, from appointment to appointment. We all know our training, and we all know we want to be the best, so let’s continue to follow through with the level professionalism we were taught! Once we have updated the health history form, it is then vital to have the current date and a new signature.
Earlier, simplicity was “promised.” Many methods can be utilized when updating the medical history. At the office I practice, we have a signing pad that connects to a USB port on the computer; Eaglesoft is our software; the customer support team can assist in setting this device up for your office. If another software is utilized in your office, it would be suggested to contact their support team to see if this can work for your office set up. I have also witnessed another office that had a computer near the front desk, and they asked patients to review the health history before the hygienist calls the patient back for their appointment. Of course, hygienists still must make it their responsibility to review this new information to be sure all new conditions are noted properly.
If you still use a paper chart, a suggestion is to ask the patient to review their previous form and make any corrections with their initials next to the correction and be sure to sign and date near the prior signature. In the past when a paper chart was utilized, it got to the point of disaster after a number of visits; at that point, it would be wise to have the patient or caregiver update a new form. This point was made very clear in the simulated court case class at the RMDC, as the dentist on trial had not shown validity in the medical history update, and the prosecuting attorney proceeded to come back to the update of the medical history time and again. When all else fails, and you need that health history done yesterday, try helping your patient complete the form, or ask another team member to assist them after their appointment with a new update. Think outside the box to manage your appointment to efficiency.
What should we be updating on health histories?
I do not believe that it is enough to simply say, “Have you had any changes in your health history?” I can tell you that so many people over the years feel that this is the time to tell me what is hurting in their mouth! No, no, no! As a veteran hygienist, I have learned how to approach certain things in a fashion that can reign in exactly for what I am looking. The verbiage I find to work effectively is, “Mr. Jones, have you had any changes in your health history since I saw you last? We last saw each other February 2016. Any new medications? Any hospitalizations/surgeries? Any new diagnoses?”
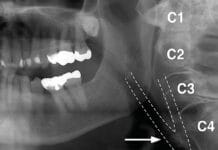
Another point made in the RMDC class was that we should be asking all of our patients is their tobacco/alcohol/drug use. In the case presented, the patient was a known tobacco chewer and alcohol user, who eventually died in his thirties of oral cancer. The doctor had made notes of hyperkeratosis on the labial mucosa of lower anteriors at several visits but failed to continue to update his usage of his habits that increased his risk factors to cancer. This was shown to be very detrimental to the dentist’s case.
Once you have asked these questions, now is the time to take control of this discussion. Otherwise, you will hear about every bowel movement, blue pill, and sniffle that has occurred since that last visit! No lie! You all know this is the straight up truth! Been there done that, right?! Let’s break this down. My recommendation is to review the last medications you had listed, delete (if computerized) or draw a line (if using a paper chart) through any discontinued meds and add any new medications. If your patient carries a list, take a copy to scan into or place in the chart. Make a big deal of patients carrying a list of medications; this makes life easier for you at each appointment and helps if a patient is in an emergency situation in everyday life. DO NOT allow your patient to say it is the same as the last time. More times than not, they have been prescribed something new that you will not learn about until halfway through the appointment, when you ask if they have an increase in dry mouth or you notice exorbitant amounts of bleeding, only to learn that they are now on a blood thinner or high blood pressure medication.
New diagnoses are a huge piece of the medical/dental puzzle that we MUST pay attention to always. When I graduated dental hygiene school in 1996, we were not being taught much in regards to talking about the oral-systemic link. Hygienists, we are smart, and we have a plethora of information to share! It is our job to know EVERYTHING, right?! Or at least we like to think so. Knowing what is going on with our patient’s overall health lays out the roadmap for our hygiene appointment.
Once a patient has indicated they have been diagnosed with Type 2 diabetes, you better believe that I am going to take time to discuss how it affects the periodontium and vice versa, as well as how people with diabetes are prone to rampant caries. You better believe that I am going to assess for dry mouth and make appropriate recommendations. With diabetic patients, it is very important to ask their A1C level at each appointment as well. Without this valuable information, hygienists are less effective within their hygiene appointment. It’s like playing catch up the entire appointment; you are grasping at straws trying to understand what has gone awry since you last saw Mr. Jones. He used to be so clean and healthy, but today his gums are bleeding like crazy, and he has dry mouth up the wazoo, with five new cavities. We are all guilty of this, but we can make a change for our patients by playing detective up front, then spending the time to discuss recommendations while we are completing their appropriate recare therapy; this approach also allows for making your life much simpler.
Sometimes we find out that our patient has a heart attack recently or had a joint replacement during the update; now is the time for a medical consult. Without this knowledge, we put patients at risk for infections that are unnecessary. Does this take extra time? Yes, this does, unfortunately. Perhaps you might train front desk personnel on the proper verbiage to use when contacting a medical office regarding something of this nature so that you can work on radiographs and get an exam while you await a response to the inquiry. If this is not an option, then inform the patient of how important it is to give them the best care possible, and you need to consult their physician before you further proceed with any treatment that could put them at risk for infection. The word infection alone alerts the patient to the importance of that phone call.
One particular matter that has become a pet peeve within this topic is that dental hygienists are not the only healthcare provider in the office who should care whether there has been a change. Dentists, if you are reading this article, please, please, please, please, please update your patient’s health histories in your treatment room. How many times are you seeing patients who have not been in for quite some time and they have an “emergency or broken tooth?” Too many to count, I would presume. If these patients have not seen your hygienist recently, guess what? Their medical history is not updated unless YOU or your assistant(s) are updating this information. Quite frankly, I am going out on a limb saying this, but I believe that the licensed individual needs to do this aspect of care or at least make sure it was done properly.
Health histories themselves are far from simple; they are quite complex because the human body is intricately designed. As dental professionals, we know that the mouth is attached to the head, that is attached to the body. By mainstreaming and controlling this brief moment in our patient’s appointments, we are able to be the absolute best provider possible for our patients. Gathering all pertinent information from the get-go helps to guide the remainder of our appointment. Do we need radiographs more frequently for our diabetic, xerostomic patient, or our recently diagnosed Sjogren’s patient who has ALWAYS had decay? Possibly. Would we rather get all of our data gathered earlier rather than later in our appointments? Yes, every single one of us wants exactly this, correct? This is because that is our right of passage as perfectionistic dental hygienists.
As our profession continues to gain strength in being more fully respected and recognized throughout the healthcare industry, something as simple as a health history update will portray each and every one of us as the professionals we expect to be treated like.
I would highly advise any dental professional to attend a course similar to that of which I attended at the RMDC. I feel the information presented is unprecedented and some of the most informative of my almost 22-year career. I could have only hoped to have had this information years ago.