Panoramic (PAN) and three-dimensional radiographs such as cone beam computed tomography (CBCT) provides invaluable information for clinicians for various reasons. These types of imaging can be utilized daily for many kinds of dental practices, including general dentistry, endodontics, periodontics, oral surgery, dental imaging centers, and orthodontics.
PAN and CBCT images provide not only an enormous amount of dental information but also a patient’s overall health. They have the potential to alert the dental professional to a potentially life-threatening condition: carotid artery disease.
Carotid Artery Disease
Carotid artery disease (CAD) occurs when the arteries that supply blood and oxygen to the brain become clogged and/or narrowed due to plaque buildup within the artery. If left untreated, it can lead to debilitating consequences and, in some cases, death by way of a stroke. Stroke is a leading cause of death and permanent disability in the United States.1
It is important to note that this complication can occur in any artery of the body, but this article will focus on the carotid due to its clinical significance for dental professionals.2
Signs, Symptoms, and Complications of Carotid Artery Disease
In the early stages, carotid artery disease may not display any obvious signs or symptoms. As the disease progresses and becomes more severe, it can lead to either a transient ischemic attack (TIA) or a stroke. Both of these complications cause a temporary loss of blood flow to the brain. The signs and symptoms of both a TIA and stroke are identical, but with a TIA, symptoms may last up to 24 hours and usually don’t cause permanent damage.3,4
In contrast, a stroke lasts longer, and the complications can be long-lasting and, in some cases, permanent. However, it is important to know that one in three people who experience a TIA will eventually have a stroke. Of the people who experience TIA and go on to have a stroke, about half occur within a year after the TIA.1,3,4
The symptoms for both TIA and stroke can include sudden weakness of limb(s), the face (usually affecting only one side of the body), speech difficulty, vision disturbances, confusion, and a sudden, severe headache.1,3,4
Any of the above symptoms are cause for concern and require immediate emergency medical attention.3
Risk Factors and Treatment
There are many risk factors for carotid artery disease, which can include diabetes, high blood pressure, high cholesterol and triglycerides, obesity, sleep apnea, sedentary lifestyle, family history and genetics, and a high-fat diet.1,3,4
Treatment of carotid artery disease depends upon the severity of the disease. Evaluation for potential carotid artery disease can include a combination of:5
- A physical exam where the treating physician evaluates the carotid artery for a “bruit,” which is commonly described as a “whooshing” sound and can indicate a blood flow issue
- Ultrasound, CT, or MRI scan
- A more detailed image, called an angiography, where a contrast dye is used in combination with either a CT or MRI to allow for a detailed image of the neck and brain
Many times, if the artery is narrowed by less than 50%, it can be treated with medications and lifestyle changes. These adjustments may include smoking cessation, implementing an exercise regime, limiting sodium intake and high-fat foods, medications that lower blood pressure and cholesterol, and antiplatelets.4
Medication or surgery may be used to manage the disease if the artery is narrowed between 50% and 70%. If the patient has symptoms with narrowing between 50% and 69%, more aggressive treatment such as surgery may be required over medication alone. Surgery is usually the first line of treatment in individuals with carotid narrowing of more than 70%.4
If surgery is determined to be the best course of action, the intervention most often used is a procedure called carotid endarterectomy. During this procedure, a surgeon makes an incision in the neck and cleans out and removes any plaque buildup clogging the artery.4
If a patient is unable to have a carotid endarterectomy, another surgical intervention called carotid angioplasty and stenting procedure may be performed. During this surgery, a catheter is placed inside a blood vessel in the groin and is threaded up to the carotid artery. A balloon is then placed inside the artery and used to widen it so that a mesh stent can be placed inside the artery. The stent keeps the artery open and allows for adequate blood flow to the brain.4
The treating physician will determine the percentage of narrowing and the severity of the disease, as well as the best course of treatment.4
Panoramic Radiograph versus CBCT
A PAN radiograph is a two-dimensional image, and a CBCT is a three-dimensional image. A PAN used to be used more frequently than three-dimensional imaging in dentistry, but CBCT has continued to gain popularity over recent years. Part of this is due to the fact that there are limitations to two-dimensional radiographs. For example, images may be enlarged, distorted, and superimposed. A CBCT image’s accuracy is much higher than a PAN image because it utilizes more precise three-dimensional technology.6
While CBCT provides more valuable information, it does expose a patient to a higher level of radiation than a PAN, so the clinician should always weigh the risk versus benefit for the patient and limit a patient’s radiation exposure.6
Clinicians should adhere to the ALARA principle (“As low as reasonably achievable”) when determining which dental images they will utilize.7,8
Identifying Potential Carotid Artery Disease on Dental Images
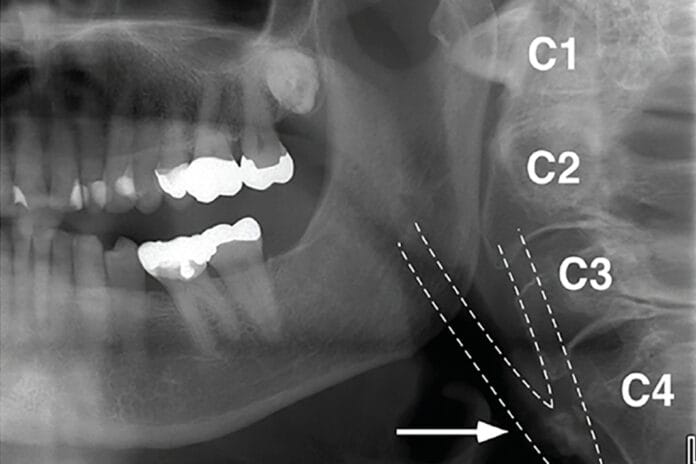
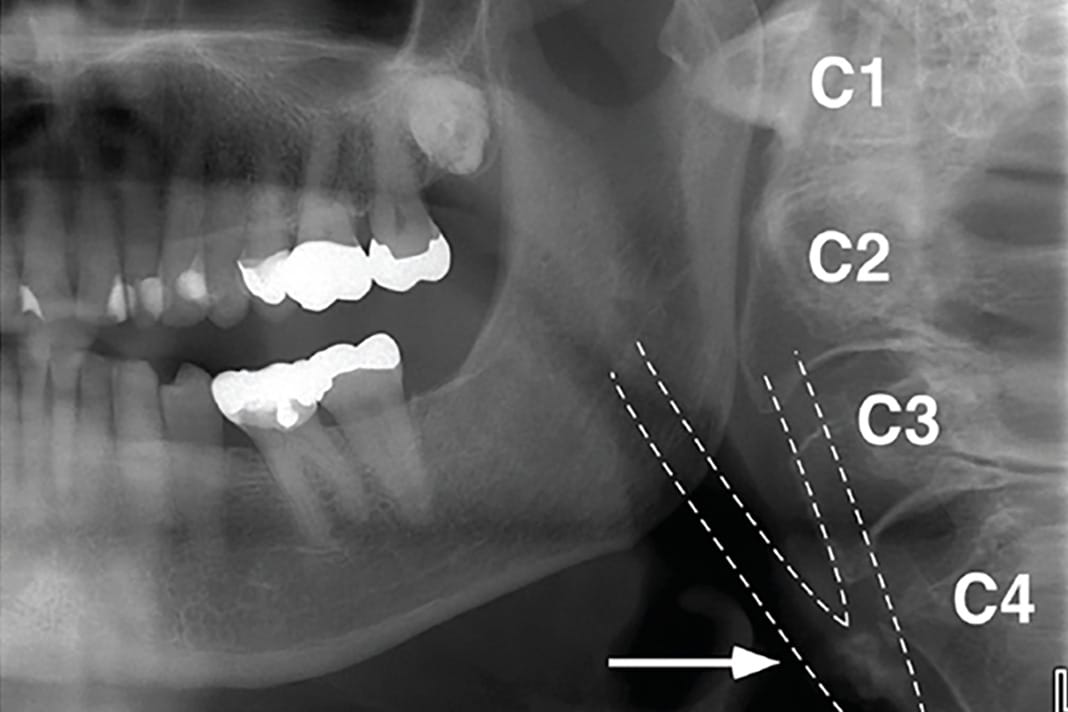
On a PAN, carotid artery calcification (CAC) can appear as a radiopaque lesion that is either rounded or nodular in shape (see Images 1 and 2).9,10 CACs most often present themselves between the C3 and C4 vertebrae. They can be localized to one side or appear bilaterally.10 Moshfeghi et al. stated, “Panoramic radiographs may help us to detect CACs in patients with or without other associated risk factors.”10 This means dental hygienists may be the first ones to discover these in their patients.

area of the carotid bifurcation in a 78-year-old female patient. Image courtesy and used with permission from Kalid Aziz, DDS, MS, and Lucinda J. Lyon, RDH, DDS, EdD.9
While CACs can be identified on a panoramic image, they are even more identifiable on a CBCT due to their high level of detail. Small calcifications are easier to identify on a CBCT scan than PAN or intraoral radiographs.11
In these images, CACs most commonly appear in the cervical tissue. From the axial view, they can be described as “single or multiple “rice grains” with a homogeneous opacity and a linear or curvilinear shape.” They appear “approximately 0 to 10 mm anterolaterally to the anterior tubercle of the transverse process; lateral or more often lateroposterior to the greater cornu of the hyoid bone; and always posterolateral to the pharyngeal airway space. In coronal projections, CAC depiction appears lateral to the anterior tubercle of the cervical vertebrae. On the sagittal sections, CACs are identified medial and inferior to the angle of the mandible, lateral and mostly anterior to the cervical tubercle with their vertical position varying from C3 to C5.”12
For an example of what a carotid artery blockage looks like on a CBCT, see Figures 1 and 2 here.12
Any of these dental images has the potential to be life-saving screenings for our patients.
Role of the Dental Hygienist
As dental hygienists, we are experts not only in oral health but the association between oral and systemic health. All of our patient’s health histories are important, but when considering our patients’ risk for carotid artery disease, those who have a history of carotid artery disease, hypertension, or diabetes, and patients taking cholesterol medications should alert us to be on the lookout for potential CACs on their dental images.
Hygienists are known for their keen eye and attention to detail, both of which can be life-saving. Identifying potential carotid artery disease on a patient’s radiographs is just one example of this. The entirety of a PAN or a 3D image should be carefully evaluated – this evaluation is not limited to the teeth only. Looking at the entire “picture” can alert the clinician to potential dangers.
If any lesion is found on a PAN or CBCT, the patient should be referred to their primary care provider or other pertinent health care physicians for an evaluation. It would be helpful to send a copy of the image to the provider so that they know exactly what the patient is being referred for.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Mayo Clinic Staff. (2023, April 19). Carotid Artery Disease: Symptoms and Causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/symptoms-causes/syc-20360519
- Mayo Clinic Staff. (2024, September 20). Arteriosclerosis/Atherosclerosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569
- Transient Ischemic Attack (TIA). (2024, February 9). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/transient-ischemic-attack/symptoms-causes/syc-20355679
- Carotid Artery Stenosis. (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/carotid-artery-disease
- Mayo Clinic Staff. (2023, April 19). Carotid Artery Disease: Diagnosis and Treatment. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/diagnosis-treatment/drc-20360527
- Acar, B., Kamburoglu, K. Use of Cone Beam Computed Tomography in Periodontology. World J Radiol. 2014; 6(5): 139-147. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4037540/
- Dental Cone-Beam Computed Tomography. (2020, September 28). U.S. Food & Drug Administration. https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/dental-cone-beam-computed-tomography
- Dental Radiographs Benefits and Safety. JADA. 2011; 142(9). https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/for_the_dental_patient_sept_2011.pdf
- Kalid, A., Lucinda, J.L. Identifying Carotid Artery Atheromas on Pantomographs. The Journal of Multidisciplinary Care. 2017; 3(9): 42-45. https://decisionsindentistry.com/article/identifying-carotid-artery-atheromas-pantomographs/
- Moshfeghi, M., Taheri, J.B., Bahemmat, N., et al. Relationship Between Carotid Artery Calcification Detected in Dental Panoramic Images and Hypertension and Myocardial Infarction. Iran J Radiol. 2014; 11(3): e8714. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4341178/
- Kumar, M., Shanavas, M., Sidappa, A., Kiran, M. Cone Beam Computed Tomography – Know its Secrets. Journal of International Oral Health. 2015; 7(2): 64-68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4377156/pdf/JIOH-7-64.pdf
- Damaskos, S., Aartman, I.H.A., Tsiklakis, K., et al. Association Between Extra- and Intracranial Calcifications of the Internal Carotid Artery: A CBCT Imaging Study. Dentomaxillofac Radiol. 2015; 44(5): 20140432. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4628503/











