The vast majority of dental hygienists are familiar with melanoma and how devastating it can be to the skin and various other organs, but how familiar are we with how it can affect the oral cavity?
Oral malignant melanoma represents a low percentage of all melanomas (thought to account for less than 1%). However, this variant tends to be more detrimental and lethal than its skin melanoma counterparts.1 Oral melanoma is extremely dangerous, so dental hygienists should be closely watching patients for any signs of malignancy.2
Oral Malignant Melanoma Prognosis
Due to its varying clinical appearances, oral malignant melanoma often goes undiagnosed until it is in its later, more advanced stages. This delayed diagnosis contributes to the overall poor prognosis for patients.3 According to the Oral Cancer Foundation, the average survival rate is estimated at less than two years.3 The Foundation also maintains that oral melanoma appears to spread more aggressively and rapidly compared to its other malignant counterparts.3
It is important to note that the American Joint Committee on Cancer (AJC) has not yet established staging guidelines on oral malignant melanoma. This is thought to be because the lesions are considered rare, and research is continually ongoing.2,3
Oral Malignant Melanoma Risk Factors
It is thought that oral melanoma mimics the pathogenesis that neoplasms found on the epidermis follow, which is by way of the basal layer of the squamous epithelium.3 In other words, the cancerous process is the same for both the oral and skin forms of melanoma.
While some risk factors for skin melanoma can be readily identified (such as UV exposure), there do not appear to be any easily identifiable risk factors for oral melanoma.3
The Oral Cancer Foundation maintains that males over the age of 40 are the most at risk for developing oral malignant melanoma. The average age of diagnosis is between 55-56.2,3 According to the Foundation, people of Japanese descent are more prone to developing this type of cancer compared to other ethnicities.3
Varying Clinical Appearances of Oral Malignant Melanoma
Oral malignant melanoma can most commonly be found on the maxillary attached gingiva and hard palate. Although less frequent, these lesions can also be located on the floor of the mouth, mandibular attached gingiva, and buccal mucosa.2-4
It is important to note that while the neoplasms are thought to arise from melanocytes, both the keratinized and nonkeratinized tissue can be afflicted by oral melanoma.5 This is important for dental hygienists to understand so that we don’t get “boxed in” thinking that these neoplasms can only occur on certain types of tissues.2-4,6
As previously stated, the clinical presentation of these neoplasms can vary greatly. The lesions range in color from brown, blue, and black. In very rare cases, the lesions have no detectable color.2,3
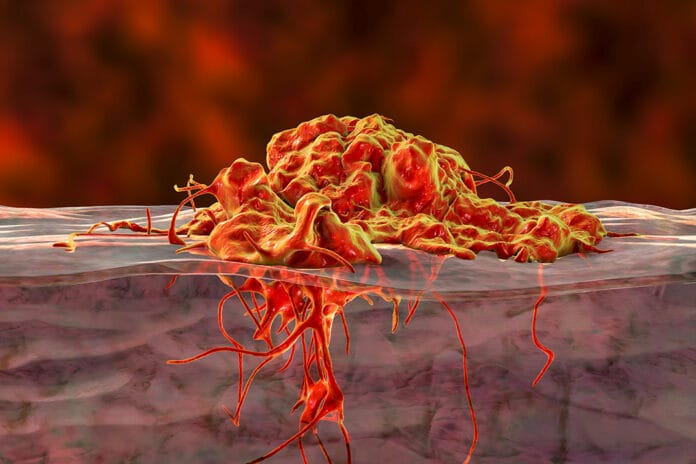
These lesions can display a great variance in their clinical presentation. They may present themselves as either a singular lesion or several lesions and can be flat or raised. They can range in color from dark brown, blue, or black. The lesions can appear as macular or elevated, and if the lesion is at a more advanced stage, it may have areas that are ulcerated.3 For a visual of what oral malignant melanoma may present as visually, please see images here.
Oral Malignant Melanoma Treatment
Due to its rare occurrences and the fact that it is often caught in its later stages, the main treatment for oral malignant melanoma is surgical excision.3 Chemotherapy, immunotherapy, and radiation can also be used in conjunction with surgical treatment if deemed necessary to prevent a recurrence.2 If the cancer has metastasized, it is considered “incurable,” but the above-mentioned treatment modalities can be utilized as needed for palliative care.2
Research is still ongoing for the best treatment modalities for oral malignant melanoma.
Early Detection is Key
As stated earlier in the article, the Oral Cancer Foundation maintains that there is a median survival rate of less than two years for patients found to have oral malignant melanoma.3 While these statistics do not offer a lot of hope, it is thought that if oral melanoma lesions are caught in their initial stages, the cancer is nearly 100% curable by excision.3
One case study stated, “Clinicians must carefully examine the oral cavity, and any growing pigmented lesion must be biopsied.”6 Another article that emphasizes the importance of early detection of oral malignant melanoma due to its high mortality rate states, “… the importance of early detection and diagnosis which can be lifesaving cannot be overemphasized.”2
We can understand that patients may not like to hear that you’ve found a suspicious lesion, or they may dislike the thought of being referred to another specialist for a biopsy that may be an additional cost to them. But when it comes to oral malignant melanoma, to put it simply, it can be a life-or-death situation.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Mazzoni, T., Zito, P.M. (2023, April 10). Oral Melanoma. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513276/
- D’souza, J., Padhye, A. Oral Malignant Melanoma: A Silent Killer? J. Indian Soc. Periodontol. 2011; 15(4): 425-428. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3283947/
- Collins, B., Abernethy, J., Barnes, L. (n.d.). Oral Malignant Melanoma. The Oral Cancer Foundation. https://oralcancerfoundation.org/facts/rare/oral-malignant-melanoma/
- Gamel, R., Madi, M., Mahmoud, M.M. Uncommon Clinical Presentation of Oral Malignant Melanoma. Beni-Suef Univ. J. Basic Appl. Sci. 2018; 7(2): 220-222. https://www.sciencedirect.com/science/article/pii/S2314853517303992
- Groeger, S., Meyle, J. Oral Mucosal Epithelial Cells. Front. Immunol. 2019; 10: 208. https://www.frontiersin.org/articles/10.3389/fimmu.2019.00208/full
- Ebenezer, J. Malignant Melanoma of the Oral Cavity. Indian J Dent Res. 2006; 17(2): 94-96. https://pubmed.ncbi.nlm.nih.gov/17051877/