As a prophylactic or treatment measure, antibiotics are prescribed in dental practices. However, a lack of knowledge regarding the choice of antibiotics or the indication for prescribing can lead to misuse and unnecessary antibiotic prescribing, contributing to the global problem of antibiotic resistance. The World Health Organization has declared this issue as one of the top ten global public health threats facing humanity.1
A study aimed to evaluate the knowledge of Jordanian dentists and assess their antibiotic-prescribing practices to identify factors contributing to inappropriate and unnecessary antibiotic prescribing. For example, prescribing antibiotics due to patient pressure and lack of consistency across different organizations’ prescribing guidelines.1
This study may have relevance to the United States and elsewhere because it was found that “39% of surveyed dentists reported that they rarely prescribed antibiotics.” However, “in comparison, other studies have shown that dental professionals were among the highest to prescribe antibiotics. In the United States, dentists were the third highest prescribers of antibiotics in the nation by volume, and they were responsible for 10% of all antibiotic prescriptions in England.”1
The Study
The study population included 345 dentists, with a majority being females who practice general dentistry. It was conducted using a questionnaire-based cross-sectional observational design, with data collected between January 2020 and June 2021.1
Researchers evaluated dentists’ confidence in their knowledge and prescribing practices. Over half of the study population felt confident about their knowledge and practice in the area of antibiotic prescribing.1
The study also provided information on the systemic diseases and conditions for which dentists prescribed antibiotics prophylactically, the procedures that prompted antibiotic prescriptions, the reasons for prescribing antibiotics, and the typical duration of antibiotic use when indicated. The most commonly prescribed antibiotics were amoxicillin, metronidazole, clindamycin, and amoxicillin/clavulanic acid.1
The Results
In this study, the researchers found that a significant portion of dentists reported prescribing unnecessary antibiotics. Specifically, 15.7% prescribed them more than once a week, 13.6% once a month, 39.1% rarely, and 31.6% never prescribed unnecessary antibiotics. Additionally, 33.9% of dentists reported feeling pressured by patients to prescribe unnecessary antibiotics more than once a week, and 31.9% experienced this pressure at least once a month.1
Gender differences were observed in reporting patient pressure to prescribe antibiotics when not medically necessary, as well as in the practice of prescribing unnecessary antibiotics upon patient request. The study also explored the relationship between the frequency of refusing patient requests for antibiotics and the number of years in dental practice (see Figure 1).1
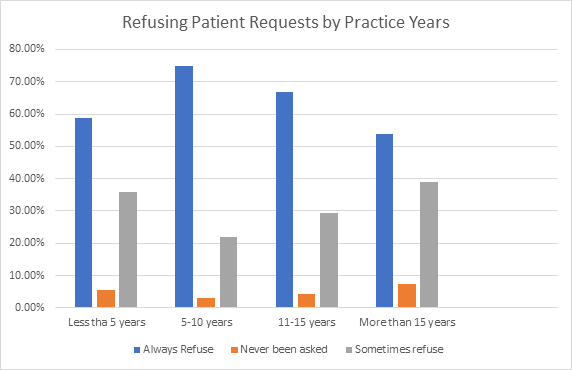
Adapted from Al-Khatib, A. & AlMohammad, R.A.1
Dentists’ perspectives on why patients might request antibiotics when they are not medically indicated were examined (see Figure 2). About 53.6% of the surveyed dentists, with variations between genders (72.0% of males and 44.1% of females), felt confident in their knowledge and practices related to antibiotic prescribing.1
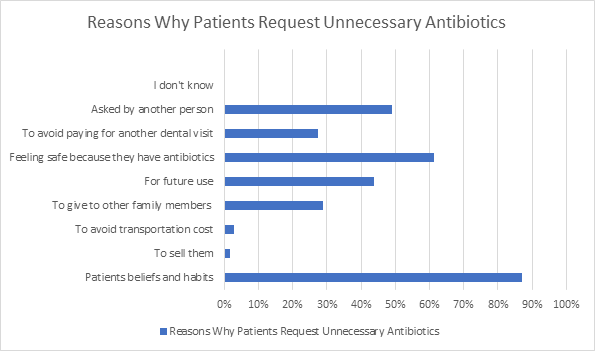
Adapted from Al-Khatib, A. & AlMohammad, R.A.1
The current guidelines on antibiotic prophylaxis for preventing infective endocarditis show variations, and they suggest that only a few specific patient groups should receive antibiotics before dental procedures. This study found that a history of infective endocarditis and the presence of a prosthetic heart valve were the most common reasons dentists prescribed antibiotics for prophylaxis. Similar practices were reported in the United States and other studies.1
However, the National Institute for Health and Clinical Excellence (NICE) guidelines no longer recommend routine antibiotic prophylaxis for dental procedures to prevent infective endocarditis. In contrast, the American Heart Association (AHA) and the European Society of Cardiology (ESC) recommend it for specific high-risk patients. This disagreement reflects inconsistent antibiotic prescribing practices and a lack of consensus in the guidelines.1
In the case of prosthetic joint patients, the American Dental Association (ADA) guidelines suggest that antibiotics are generally not needed before dental procedures, but some dentists still prescribe them, even though most experts advise against it.1
Conclusion
Antibiotic overprescribing occurs when antibiotics are used unnecessarily, even for infections that can be managed without them. This can happen in cases of uncomplicated cellulitis with unnecessarily long antibiotic courses. Recent studies and guidelines suggest that antibiotics should not be routinely prescribed before various dental procedures, including restorative treatment, simple root canal treatment, tooth abscess treatment, tooth preparation for prosthetics, routine hygiene treatment, orthodontic bracket placement, anesthesia administration, and radiographs.1
Overprescribing antibiotics carries significant long-term risks, including life-threatening diseases, opportunistic infections like Clostridium difficile, more adverse events, higher complication risks, increased mortality rates, more hospital admissions, and the development of antibiotic resistance. Dentists and patients both play essential roles in combating antibiotic resistance, making it crucial to understand dentist prescribing habits and the influence of patient requests for antibiotics on those habits.1
The study concluded that antibiotic prescribing practices among dentists are not consistent with current guidelines, and unnecessary antibiotic prescribing can be influenced by patient pressure. To address this issue, the researchers suggest updating and clarifying guidelines, restricting antibiotic use to cases where the benefit outweighs the risk of harm, prohibiting over-the-counter antibiotic availability (in countries where this is available), educating dentists on how to respond to patients’ requests for antibiotic prescriptions, and implementing antibiotic stewardship practices and programs.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on pure education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
Reference
- Al-Khatib, A., AlMohammad, R.A. Dentists’ Habits of Antibiotic Prescribing May be Influenced by Patient Requests for Prescriptions. International Journal of Dentistry. 2022; 2022: 531873. https://doi.org/10.1155/2022/5318753











