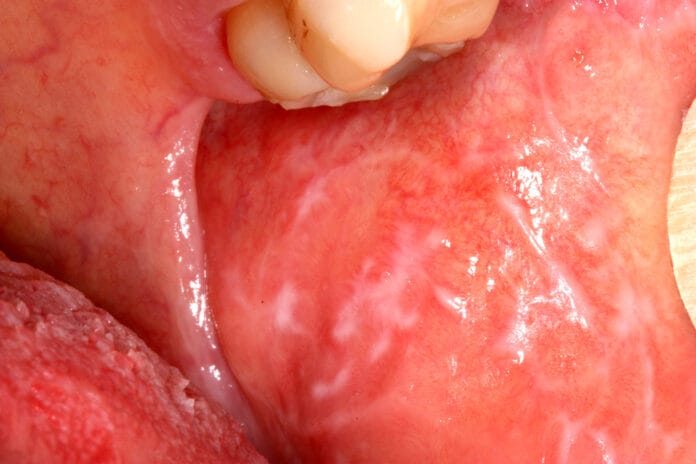
Oral lichen planus is a chronic inflammatory disease that affects mucous membranes. Patients with oral lichen planus may be at risk for oral cancer in affected areas. Lesions are most often seen on the buccal mucosa, tongue, gingiva, and palate.
Lichen planus can appear as lacey white raised patches, red swollen patches, or ulcers. White lacey patches may not cause discomfort. However, red patches and ulcerated lesions often do, which may hinder speaking, eating, drinking, and oral hygiene habits. Topical steroids may help but, unfortunately, may also cause candidiasis. A recent study used a topical steroid, fluocinolone acetonide 0.1% in orabase, to treat oral lichen planus, and examined whether any changes occurred in the patient’s oral biome.
Background on Oral Candida, Lactoferrin, and Topical Steroids
Topical steroids are immunosuppressive, and while they provide relief for oral lichen planus lesions, they also create an environment for virulent oral microbes to thrive. Normal amounts of Candida exist in healthy patients and can be found in about half the population. However, an overgrowth leads to candidiasis (yeast infection), further aggravating oral lesions, thus creating a painful cycle for oral lichen planus patients.
In addition to oral Candida levels, researchers were interested in the patient’s salivary lactoferrin levels since these glycoproteins inhibit microbial growth in two potential ways. Lactoferrin binds to salivary iron, hence creating an iron-deficient environment that hinders microbial growth and permeates fungal cell walls, leading to cell death. Prior studies found a negative correlation between salivary lactoferrin levels and Candida overgrowth, so this study paid close attention to their levels as oral lichen planus patients treated their oral lesions with a topical steroid.
The Study
This study included 15 oral lichen planus patients recruited from Chulalongkorn University’s Dental Hospital in Thailand, consisting of 13 female and two male subjects, with an average age of 48 years old. In comparison, a test group of 15 healthy patients, all female, averaged 54 years old. Patients had no prior signs or symptoms of an oral yeast infection, no medical predisposition to yeast infections, and no history of using antifungal agents. Also, participants did not smoke for at least a month before the study, nor did they use an antiseptic mouthwash. Researchers were blinded in order to prevent bias.
Saliva samples determined the subject’s salivary flow rate, lactoferrin concentration, salivary lactoferrin flow rate, oral Candida colonization, and the oral Candida species. All participants refrained from eating and drinking for at least two hours before providing their saliva samples.
After the initial sample collection, the study group proceeded to use fluocinolone acetonide 0.1% in orabase three times a day for three months. After treatment, the study group provided another saliva sample.
Results
Researchers evaluated three sets of saliva samples: one from healthy subjects, and two from oral lichen planus patients, before and after topical steroid treatment. Oral Candida was found in 11 healthy subjects, eight patients before topical steroid treatment and nine patients after treatment, but there wasn’t much difference in Candida counts between the groups.
Overall, this study found that treating oral lichen planus lesions with topical steroids during a three-month period did not cause any significant changes in salivary lactoferrin or oral Candida levels. Similarly, no significant changes were found between each group’s salivary flow rates, lactoferrin concentration, salivary lactoferrin flow rates, and oral Candida colonization.
When investigating possible relationships between oral Candida, salivary flow rates, and lactoferrin, there was no significant relationship between oral Candida and lactoferrin in the sample groups. However, there was a negative correlation between oral Candida levels and salivary flow rate in both the control group and the oral lichen planus patients before topical steroid treatment, likely because a higher salivary flow rate increases oral flushing actions, hence discouraging microbial colonization.
This study did not find any significant relationship between salivary flow rates and lactoferrin, even though previous research found that lower saliva levels correlate with lower lactoferrin levels. However, this study did find a lower lactoferrin concentration and lactoferrin flow rate in oral lichen planus patients after treatment compared to other samples, but this finding was insignificant.
These results are promising for oral lichen planus patients, but further studies with a larger subject pool over a longer period of time are recommended.