Patient safety and infection control are top priorities for hygienists. Surprisingly, there are many dental offices that do not adhere to the latest safety and infection control protocols. Some dental professionals continue to use outdated or ineffective infection control methods because they have always used them, while other dental professionals simply skip over required infection control training.
Below are five infection control mistakes you could be making without realizing that you are endangering patients and fellow staff.
Mistake #1: Failing to sterilize slow-speed handpieces between each patient.
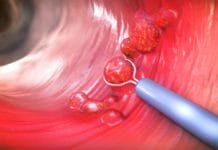
Many people assume that they can disinfect slow-speed handpieces with a surface disinfectant because slow-speed handpieces are categorized as semi-critical devices. Unfortunately, this is not the case. According to the Centers for Disease Control and Prevention (CDC), handpieces should be treated differently than the majority of semi-critical devices. The CDC states, “Studies have shown that handpieces can become contaminated internally with patient materials and the next patient may be exposed to potentially infectious materials (2,3,5).”
- Future patients may be exposed to infectious materials if handpieces are not sterilized. (2,3,5).
- The CDC states that handpieces should not be used unless they can be heat-sterilized
- Accordingly, hygienists should not use handpieces that cannot be removed from the dental unit. (7).
Compliance with CDC recommendations is best achieved by purchasing multiple handpieces to allow time to sterilize each handpiece between every patient. Offices who are reluctant to invest in extra handpieces due to cost should remember that infection control and patient safety are top priorities, and buying multiple handpieces is the cost of doing business.
Mistake #2: Assuming that all disinfectant wipes are created equal.
To properly disinfect a clinical contact area, the surface must first be wiped clean of blood, saliva, bioburden, and other debris. Only then can successful disinfection occur. The method wipe, discard, wipe means to make the first pass to clean surfaces, then a new wipe is used to disinfect surfaces. Two passes are necessary because the failure to fully remove debris during cleaning can hinder the disinfecting process, nullifying the effectiveness of the disinfectant. To thoroughly clean a surface, the CDC requires the following:
- Use of a low-level EPA-registered hospital disinfectant for general cleaning (if blood is not present)
- Application of an intermediate-level cleaning product with a tuberculocidal claim to clean blood (2,7)
- “Not all disinfectant products should be used as cleaners unless the label indicates the product is suitable for such use (2)”
When selecting a cleaning agent, clinicians should consider both the product’s ability to clean and the product’s alcohol content. This is because alcohols are poor cleaning agents in the presence of organic materials and can be rendered ineffective when organic materials such as blood and saliva are present (1). These agents have difficulty penetrating bacterial spores and other protein-rich materials. “Following exposure to alcohol, denatured bioburden becomes more insoluble and tenaciously adherent onto most surfaces (9).” Hence, water-based cleaners are better than alcohol-based cleaning agents (1,9).
This mistake can be avoided by simply reading the labels on the disinfectant products you use. Remember that you must first properly clean a surface before applying disinfectant products. And never assume that a product can clean just because it can effectively disinfect a surface.
Mistake #3: Placing instrument pouches in sterilizers the same way regardless of model.
It would certainly be convenient and easy to always sterilize all instrument pouches using the same procedures you learned in hygiene school. Unfortunately, sterilizers vary widely according to the manufacturer, make, and model. The chances are that your dental office will not be using the exact same model that your hygiene program used.
As a hygienist, you have a responsibility to familiarize yourself with the instructions provided by the manufacturer. Even if you think you might be using the same model sterilizer you used previously, you should still check the operator’s manual to ensure that you are using the same model. Below is a step by step process you can take to ensure that you are properly sterilizing your instrument pouches:
- First, confirm the make and model of the sterilizer you are using in your office.
- Pull the user guide that corresponds to that make and model (some offices have multiple models!).
- If you cannot find the user guide, check the manufacturer’s website to see if you can access a copy.
- Check the guide to see whether you should place pouches paper side up or down in the chamber.
- Some manufacturers recommend positioning pouches on their edge using a rack or accessory.
- Do not forget to store the operator’s manual safely for future use.
The above steps are very important to follow because sterilizer manufacturers offer a variety of differently sized sterilizers and operating procedures. Regardless of the make and model of sterilizer your office uses, there are a few key points that you should always remember about sterilizing instruments:
- Loosely packed instrument pouches promote proper steam flow and the most effective sterilization.
- Pouches should never be stacked or piled on top of each other.
- Never exceed the recommended maximum capacity outlined by the manufacturer in the user guide.
- Always let instrument pouches fully dry before you touch them. Moisture acts like a wick and can draw bacteria from the environment, your hands, or the surface they are placed on and pass through the packaging, contaminating instruments (7).
- Label instrument packages to show which sterilizer was used and the cycle/load number. Be sure to include a date on the label. This can help if there is a processing/sterilization failure (2).
With all of the different sterilizer manufacturers and units on the market, it is important to make sure that you do not operate on auto-pilot when you sterilize your instruments. One of the best ways to avoid making any sterilization mistakes is to adhere to the following recommendation provided by the CDC:
Mistake #4: Transporting contaminated instruments to the sterilization area in a cassette.
While cassettes offer an effective means of protecting and organizing dental instruments, they are not designed to transport contaminated instruments from the operatory to the sterilization area. The CDC advises clinicians to employ work-practice controls, such as carrying contaminated instruments in a covered container, to reduce the chance of exposure to harmful agents. The Occupational Safety & Health Administration’s (OSHA) Bloodborne Pathogens Standard offers further guidance for handling contaminated instruments:
“Contaminated materials that are to be decontaminated at a site away from the work area shall be placed in a durable (puncture-resistant), leak-proof, labeled or color-coded container that is closed before being removed from the work area.” (12)
A great way to avoid this mistake is to invest in instrument trays with locking covers to transport contaminated instruments from the operatory to the sterilization area. In addition to serving as an effective means of safely transporting used instruments, trays with locking covers can help protect patient care items from cross-contamination during storage.
Mistake #5: Assuming you are up to date on the latest infection control protocols because you read this article.
You’re probably really not thinking this, but it does bring me to the last point of CDC infection control requirements for training in every office. Per CDC guidelines, offices should conduct infection control training for employees that have an occupational risk of exposure, “at a minimum, annually (7).” When new employees are hired the CDC requires they should receive infection control training. “If new tasks or procedures are assigned to an employee that affect their occupational exposure” infection control training should be done as well, per the CDC (7).
Every dental office needs to have an “infection control coordinator who should be responsible for developing written infection prevention policies and procedures based on evidence-based guidelines, regulations, or standards. The infection prevention coordinator should ensure that equipment and supplies (i.e. hand hygiene products, safer devices to reduce percutaneous injuries, and personal protective equipment) are available and should maintain communication with all staff members to address specific issues or concerns related to infection prevention. Also, all dental settings should have policies and protocols for early detection and management of potentially infections persona at initial points of patient encounter (2).”
Below are a few ways to ensure that you are well-versed in the latest infection control protocols:
- Make sure that all new employees are trained on the proper infection control procedures.
- Designate an Infection Control Coordinator to ensure that employees are properly trained.
- Familiarize yourself with policies and protocols for managing potentially infectious individuals. (2).
- Maintain detailed records regarding infection control policies, immunizations, and training.
- Participate in ongoing infection control and safety training seminars at least once per year.
The Bottom Line
Reviewing and keeping your infection control protocols up to date is vital to the safety of our patients and ourselves as clinicians. Many infection control questions can be found in the CDC’s 2003 Guidelines for Infection Control in Dental Health-Care Settings (which is still current) (4). Remember to always follow manufacturer instructions and take advantage of continuing education opportunities to ensure that you remain on the cutting-edge of infection control.
READ: Part 2: 5 More Infection Control Mistakes to Avoid
Now Listen to the Today’s RDH Dental Hygiene Podcast Below:
Resources:
- Abel, S.N., et.al. (2000). Dental Alliance for AIDS/HIV Care. Principles of Oral Health Management for the HIV/AIDS Patient. Retrieved from https://aidsetc.org/sites/default/files/resources_files/Princ_Oral_Health_HIV.pdf
- Centers for Disease Control and Prevention. Guideline for Hand Hygiene in Health-Care Settings. MMWR 2002; 51 (No. RR-16). Retrieved from http://www.cdc.gov/mmwr/PDF/rr/rr5116.pdf
- Centers for Disease Control and Prevention. (2016, March). Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Retrieved from http://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care.pdf
- Kohn, W.G., Collins, A.S., Cleveland, J.L., Harte, J.A., Eklunt, K.J., Malvitz, D.M. Center for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. MMWR 2003; 52 (Report No. 17). Retrieved from https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
- Organization for Asepsis and Prevention (OSAP). Frequently Asked Questions on Dental Infection Control. Retrieved from http://www.osap.org/?FAQ_Instrum_Disinf1#ireadrecently
- Organization for Asepsis and Prevention (OSAP). Frequently Asked Questions Instrument Sterilization. Retrieved from http://www.osap.org/?FAQ_Instrum_Ster2#agraduate
- Robinson, D.S., Bird, D.L. (2013). Essentials of Dental Assisting (5th ed.). St. Louis, MO: Elsevier Saunders.
- Rutala, W.A., Weber, D.J., HICPAC. Centers for Disease Control and Prevention. (2008). Guideline for Disinfection and Sterilization in Healthcare Facilities. Retrieved from http://www.cdc.gov/hicpac/pdf/guidelines/disinfection_nov_2008.pdf
- Sears, B., Cooper, C. Younai, F.B., Donohoe, T. (2001, Dec.). The Williams Institute. HIV Discrimination in Dental Care: Results of a Discrimination Testing Study in Los Angeles County. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/Sears-HIV-Discrimination-Dental-Care-Dec-2011.pdf
- Sultan Healthcare. Retrieved from http://www.sultanresurge.com/Content3.html