Cerebrocostomandibular syndrome (CCMS) is an extremely rare disorder with a low survival rate. This condition is so rare that only around 80 confirmed cases have been reported in medical literature. The disorder involves a severely small chin, glossoptosis, an absent uvula, a cleft palate, narrow chest, missing ribs, gaps between the ribs, and difficulty breathing and feeding.1
Other conditions are scoliosis, developmental or/and intellectual delay, and hearing loss.2 CMMS may affect individuals differently.
Cerebrocostomandibular syndrome occurs randomly, often without a heredity connection. With CCMS, the gene that is changed to cause this is SNRPB. Most of the time, it’s new to a child and hasn’t shown up with other family members, although a few cases have been connected to autosomal recessive and dominant inheritance.
With the autosomal recessive, both copies of the gene in each cell must have a mutation. In these cases, the affected person inherits one mutated copy of the gene from each parent, and most likely, each parent is unaffected. In an autosomal dominant condition, one mutated copy of the gene in each cell is enough to carry signs and symptoms of CMMS.
An autosomal dominant condition may be inherited by a parent, or the mutation may occur for the first time in the affected person. This condition then gives their child a 50% risk to inherit CMMS. Males and females are equally affected.1 It has been noted that parental consanguinity has been the cause in a few cases.3
Glossosptosis − Glossosptosis is a common craniofacial abnormality in developmental disability, and, in CCMS, it plays a major role in survival. This oral condition displaces the tongue in a downward and backward position, which commonly obstructs the airway, throat, and pharynx, preventing sucking, swallowing, and feeding. An unusually smaller jaw in a CCMS patient affects the development of the palate, causing a cleft.
Early diagnosis and treatment may allow proper growth and development of the tongue. Since dental professionals may not see children within their first year of life, a medical doctor will likely be the professional to diagnose these developments. To correct these conditions, multiple specialties, including otolaryngologists, plastic surgeons, dental professionals, oral surgeons, and maxillofacial specialists, are involved. CCMS surgery is commonly needed because of the other conditions which are common with this disease. With a high success rate, glossopexy tongue surgery is a technique to place the tongue in a forward direction, clearing the airway.4
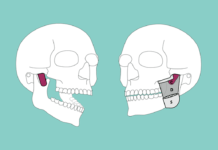
Micrognathia − Micrognathia is a facial deformity related to the development and position of the fetal mandible. It’s considered hypoplasia of the mandible, causing a small, receding chin that is frequently associated with different syndromes.
The development of the mandible is multifactorial. Maldevelopment can cause insufficient tongue growth and position, preventing lateral palatine shelves from medial migration and midline fusion, causing a significant association with micrognathia and cleft palate (both are major roles in CCMS).5
Ribs − In CCMS, the rib defects are variable in an individual. A person will tend to have large gaps between all or only a few ribs, especially in the back of the ribcage close to the spine. Typically, there are missing ribs, as twelve pairs of ribs are traditional in normal anatomy. In CCMS, there may be between seven to 11 ribs.
The lower pairs of the ribs may be underdeveloped, gapped, or completely absent. In CCMS, it is common the ribs will not connect to the spine the way they should, leading to narrow rib cages.
The narrow rib cage and small jaw concerns increase breathing and feeding challenges. The defects may or may not be symmetrical. Certain defects resemble fractured ribs that will ossify later in life, or additional bone grafts or implants may be needed.1 The severity of the rib defects seem to correlate with the severity of the overall syndrome and survival rate.1,2
Cerebrocostomandibular Syndrome Prognosis
Prognosis depends on the severity of anomalies. The most severe cases are fatal within the first hours after birth. Within the first month, 25% are fatal, and 35% die within the first year. The reason for the early deaths is insufficient oxygen intake and the inability to breathe in correlation with the tongue blocking the airway and small rib cage.1 These fatalities correlate highly with the greater amount of missing ribs or gaps between the ribs.
Individuals who survive the first year of life have less severe anomalies and commonly make it into adulthood. They may suffer from scoliosis, inhibited growth, reduced lung capacity, feeding disturbances, intellectual deficit, conductive hearing loss, language disturbances, and dental anomalies.2 Dental anomalies include micrognathia, cleft palate, and glossoptosis.
Scoliosis develops in childhood and affects 50% of people with this condition. Spinal fusion may be necessary for correction. Due to a possible lack of oxygen at birth, developmental and intellectual delays are commonplace. Development increases once the respiratory problems are conquered.1
Prenatal ultrasonic diagnosis of CMMS plays a key factor in survival. Longevity is related to early aggressive interventions and addressing major anomalies with long-term management of treatment. Many people with CCMS can live full, productive lives.1,3
Cerebrocostomandibular Syndrome Management
A multidisciplinary approach is highly recommended for proper and effective management. Clinical presentation and chest x-rays determine the diagnosis. Management includes intensive care for respiratory function, improving feeding difficulties, and recurrent infections.
The majority of treatment is needed during infancy for survival to progress into adulthood. Breathing difficulty can be fatal in childhood. Most babies within the first year of life need surgery to help them breathe and eat. These surgeries include a breathing tube directly into the throat, expansion of the jaw or chest, a feeding tube into the stomach, and cleft palate reconstruction.
During pregnancy, some features of CCMS may be seen on an ultrasound, such as micrognathia and improperly formed ribs. Most patients are diagnosed or confirmed after birth.1,3
Related Disorder: Pierre-Robin Syndrome
Cerebrocostomandibular syndrome resembles Pierre-Robin syndrome.2 The main features of Pierre-Robin syndrome are cleft palate, micrognathia, and glossoptosis. The main difference is the rib defect noted in CMMS, which is not an issue with Pierre-Robin syndrome.
Pierre-Robin syndrome may be an isolated condition or associated with other conditions. This condition is also uncommon and affects one in 8,500 to 14,000 people. It occurs equally among males and females but is more common in twins.
It’s not inherent. Usually, the person affected is the only family member to have it. A mutation of the SOX9 gene is known to be the culprit. The exact causes are unknown as to why Pierre-Robin syndrome happens. Possible causes may be a low volume of amniotic fluid limiting chin growth, weakness of the facial muscles, or a connective tissue disease.6
Pierre-Robin syndrome is also called Pierre-Robin sequence because if one developmental step doesn’t happen, the next one also doesn’t fully happen.
The first step is an underdeveloped jaw that sets off other steps in the uterus. Seven to 10 weeks into a pregnancy is when the baby’s jaw starts to grow rapidly, allowing the tongue to descend into the two halves of the palate. If the lower jaw doesn’t properly grow, the tongue prevents the palate from closing, resulting in a cleft palate. The small lower jaw causes the tongue to be positioned at the back of the mouth, causing breathing and feeding issues.
In some children with Pierre-Robin sequence, the mandible growth may develop into a normal size chin, or surgery may need to be completed. An additional symptom may be natal teeth − teeth present at birth.6,7
Since CMMS is such a rare disease, there have not been many studies or reports on the lifespan due to the lack of medical confirmed subjects. In Pierre-Robin syndrome, the life span is normal. With both syndromes, it has been reported that, if the initial conditions of breathing and feeding are resolved, many people can live full, productive lives.1,6
With such a small percentage of people with CCMS and Pierre-Robin syndrome, we most likely won’t ever treat these patients during the most severe stages of these syndromes. But it may be worth knowing if a patient has a developmental or intellectual delay with micrognathia since there may be a correlation to one of these two syndromes.
Now Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Cerebrocostomandibular Syndrome. NORD National Organization for Rare Diseases. 2019. Retrieved from https://rarediseases.org/rare-diseases/cerebrocostomandibular-syndrome/#general-discussion
- Cerebrocostomandibular Syndrome. Orphanet. May 2013. Retrieved from https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=1393
- Hosalkar, H.S., Shaw, B.A., Ceppi, C.L., Ng, B.C. The cerebro-costo-mandibular syndrome: 9-year follow-up of a case. J Postgrad Med. 200; 46(4): 268-71. Retrieved from: http://www.jpgmonline.com/text.asp?2000/46/4/268/260
- Sukanya, G. What is Glossoptosis? Characteristics and Treatment. StemJar. August 11, 2019. Retrieved from https://www.stemjar.com/what-is-glossoptosis/
- Radiology Key. Micrognathia and Retrognathia. July 7, 2019. Retrieved from https://radiologykey.com/micrognathia-and-retrognathia/
- Pierre Robin Sequence. National Institutes of Health. Retrieved from https://rarediseases.info.nih.gov/diseases/4347/pierre-robin-sequence
- Pierre-Robin Syndrome. Texas Children’s Hospital. Retrieved from https://www.texaschildrens.org/health/pierre-robin-syndrome