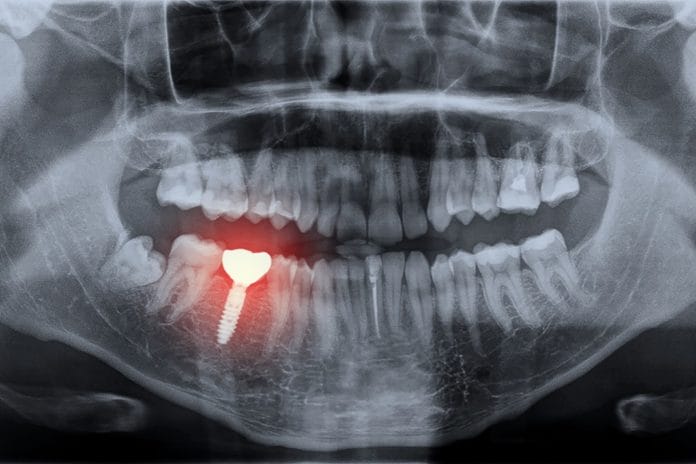
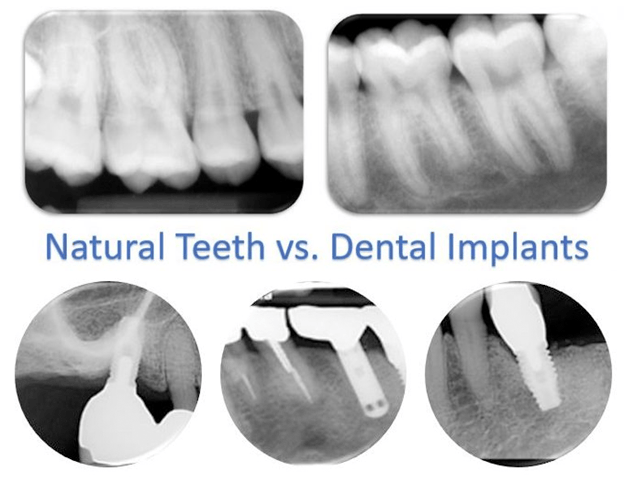
The restorations that are supported by dental implants are designed to resemble a natural dentition, but do dental implants really look like teeth? If you examine the anatomy and, in some cases, the positioning of an implant in comparison to how teeth are in the jaw, there can be major differences in respect to diameter, shape, size, contour, and even location.
Dental implants can replace a single tooth, multiple teeth, or all teeth. The restorations supported by the implants can be a single crown, multi-unit bridge, full arch bridge, fixed/removable complete and/or partial dentures. Out of the many different restorative options recommended by dentists, the best decision would be the one that is most cleansable for a professional and at-home maintenance regimen that is realistic for the patient and practitioner. Dental literature and expert clinicians agree the endpoint goal of treatment is a high aptitude for implant maintenance.1-4
Our ethical responsibility as dental hygienists is to equip this population with home care devices specifically designed for their restorative and dexterity needs. However, despite our best efforts, a poorly designed restoration is a predisposing risk factor for plaque accumulation and an environment that is non-maintainable by the patient with a regular toothbrush and floss.
When exploring the best recommendations for your patients, remember that this may challenge clinicians to step outside the box of traditional dental hygiene methodology. However, in order to do so, hygienists need to increase their knowledge and understanding of dental implant restorations and how to identify potential risk factors for disease. The following are three cases meant to demonstrate the significance of restorative design and its contribution to plaque accumulation and disease.
Significance of Restorative Design
Case Example 1: Two-unit bridge supported by two implants
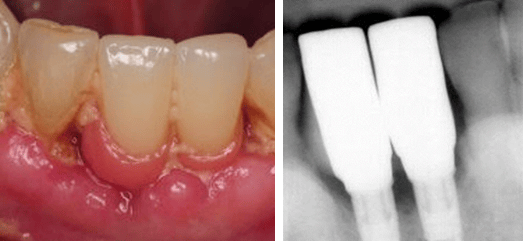
The first case example is of a two-unit implant-supported bridge in place of missing teeth numbers 24-25. There is obvious moderate to heavy plaque and food accumulation with soft and hard tissue inflammation. The implant crowns being fused together with submucosal restorative margins limits access for personal oral hygiene in all embrasure spaces, especially between 24-25. The design of the restoration also created additional spaces, especially evident where the bridge meets adjacent teeth #23 and #26.
The pink acrylic in place of soft tissue is generally convex, contributing to a bulky restorative design and a non-maintainable environment. Although many factors need to be considered as contributing to the problem, perhaps the restorative doctor could have avoided some of these complications with the recommendation of two single implant crowns instead fusing the two together.
Case Example 2: A three-unit implant-tooth supported bridge
It is widely known that dental implants lack periodontal ligaments. This is one major characteristic that sets dental implants apart from teeth. Therefore, the concept of splinting a rigid ankylosed implant to a relatively mobile tooth remains controversial.
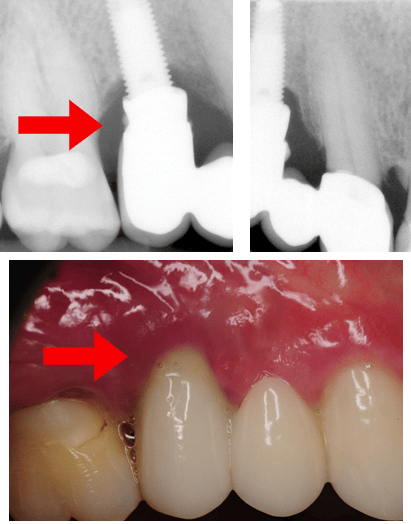
Some researchers believe “that the difference in support at both ends of the system places the implant at risk for complications.”5 This is a case example of a three-unit implant-supported bridge in place of teeth # 4-5 with obvious limitations for adequate hygiene attributable to design. When looking at the clinical image, the restoration may look appropriate, but the radiographs suggest otherwise.
Something else that needs consideration when examining dental implant restorations for hygiene accessibility is retention. This is a three-unit cement-retained implant tooth-supported bridge. Not only does the design of this bridge make hygiene challenging, but if you examine the radiograph closely, you will notice residual cement, which presents another risk factor for plaque accumulation and peri-implant disease.
Note radiographic residual cement and peri-implantitis with pus exudation.
Case Example 3
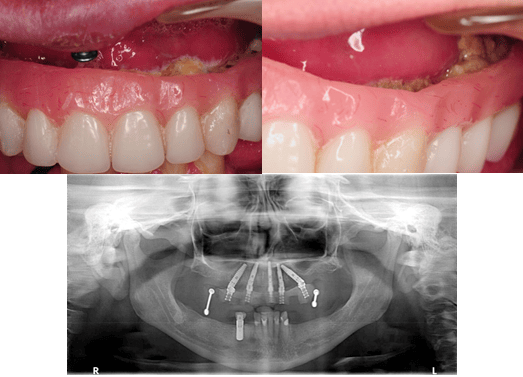
Full-arch implant therapy in a transitional denture supported by five implants
Implant dentistry is especially sought after by the edentulous population or patients with a terminally ill dentition. The transitional phase of implant therapy (where a patient is in a provisional or temporary restoration during osteointegration) is a crucial time for the patient to be seen by a dental hygienist. This will help uncover any inadequacies in restorative design that may complicate home care before the final restoration is delivered.
This case is an example of a poor transitional design that made at-home maintenance impossible for the patient. All five implants developed peri-implantitis and were removed only four months after placement.
Implant dentistry has improved the quality of life for much of the world. Regardless of how technology has advanced, peri-implant disease remains a global concern with an emphasis on maintenance.
Restorations supported by dental implants are designed to resemble a natural dentition. However, professional and at-home maintenance methods should be tailored to the design of the supporting restoration (and patient), not teeth! Coincidentally, the design of the restoration can be the major component causing the problem. Either way, it is the role of the dental hygienist to identify risk factors for disease, intervene when it is detected, and prevent it from happening!
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Nevins, M., Froum, S. (2017, June). Multidisciplinary Treatment Solutions for Peri-implantitis Symposium. Chicago.
- Monje, A., Insua, A., Wang, H.L. Understanding Peri-Implantitis as a Plaque-Associated and Site-Specific Entity: On the Local Predisposing Factors. Journal of Clinical Medicine. 2019; 8(2), 1–19. DOI: 10.3390/jcm8020279.
- Beumer, J. III, Faulkner, R.F., Shah, K.C., Moy, P.K. Fundamentals of Implant Dentistry: Prosthodontic Principles. Hanover Park, IL: Quintessence Publishing; 2015.
- Rosen, P. S., & Froum , S. J. (2018). Peri-Implant Disease: A Primer Etiology, prevention, and treatment. Inside Dentistry , 14(9). Retrieved from https://www.aegisdentalnetwork.com/id/2018/09/peri-implant-disease-a-primer
- Al-Omiri, M. K., Al-Masri, M., Alhijawi, M. M., & Lynch, E. (2017). Combined Implant and Tooth Support: An Up-to-Date Comprehensive Overview. International journal of dentistry, 2017, 6024565. https://doi.org/10.1155/2017/6024565