Oral lichenoid lesions (OLL) refer to a group of lesions that appear as white ─ or a combination of red and white ─ and can be found on multiple surfaces in the oral cavity. They often look similar (and even identical) to oral lichen planus (OLP). One article stated, “Typically, the clinical presentation in both conditions can be reticular white patches, papules, or plaques with or without erosions or ulcerated areas.”1
OLLs are most often singular in nature, which can help differentiate them from OLP and other lesions that tend to appear bilaterally or in multiple locations throughout the oral cavity. The patients with these specific lesions can be symptomatic or asymptomatic.1,2
Hypersensitivity Reaction
For a very broad and basic review of physiology, a hypersensitivity reaction happens when the body’s immune system mounts an exaggerated response to an allergen or antigen that it sees as an “invader.”
The first three of the four types of hypersensitivity reactions are Types I, II, and III. These are known as immediate hypersensitivity reactions (IHR) because the exaggerated immune response happens within 24 hours of being exposed to the allergen or antigen.3 Type IV is a delayed hypersensitivity because it can take much longer than 24 hours to respond after encountering the allergen or antigen.4
It has been determined that OLLs are not IHRs but rather manifest as “delayed,” or in other words, a type IV hypersensitivity reaction.
Reaction to an Amalgam Restoration
One specific example of a type IV hypersensitivity reaction found in the oral cavity is that of an OLL in response to a nearby amalgam restoration. Oral mucosa that comes into contact with an amalgam restoration may trigger the body to see the amalgam as “foreign” and mount an exaggerated but delayed immune response. This response can happen anywhere from 72 hours to years after the restoration has been placed.1
One article maintains that while this type of reaction is rare, the cause is almost always from the tissue coming into contact with the mercury component of the amalgam restoration.1 The article goes on to state that these lesions can be painful or sensitive, especially when they come into contact with food that may be either “spicy” or “hot.” Or, the lesion can be completely painless, and the patient may not be aware they have an existing lesion.1
As mentioned earlier, these lesions can appear as white patches or plaques that can have surface ulcerations or erosions to them and can be similar to the appearance of OLP.1
While OLLs can be found anywhere in the oral cavity, if a lesion presents as a result of direct contact with an amalgam restoration, the most common sites are the tongue and buccal mucosa.1
Lichenoid Mucositis
Lichenoid mucositis (LM) is a condition that can be described as being under the umbrella of OLLs and is also considered a hypersensitivity or allergic reaction to either dental materials (composite, ceramic, or materials other than amalgam) or as a response to a drug the patient is taking. As we know, the list of medications that can cause anomalies and side effects in our patients’ mouths is continually growing. But two of the most common drugs that can cause OLLs are nonsteroidal anti-inflammatory drugs (NSAIDs) and angiotensin-converting enzyme inhibitors (ACE).2
The diagnosis of lichenoid mucositis can be made without a biopsy if the clinician can identify the allergen or medication that is causing the LM. When the allergen (such as a ceramic crown) or medication is removed from the patient, and the lesion resolves, a diagnosis of LM can be assumed.5
Differentiating between the Lesions
OLLs cannot only mimic OLP but other oral lesions as well. These can include ones that appear as a result of certain drug reactions and different systemic diseases such as graft versus host disease and lupus.1
The main distinction between the above-mentioned disorders and OLLs is that they tend to appear in multiple areas throughout the oral cavity. On the other hand, OLLs tend to be singular and localized in nature. Since OLP can be considered premalignant, it is imperative clinicians understand these differences.1
Different Types of Biopsy Methods
Excluding a definitive diagnosis of LM, OLLs can mimic other lesions that have the potential to become malignant, so a biopsy must be performed to rule out these possibilities.
A few different types of biopsy methods can be used, and the three below are the most commonly used methods.
Excisional ─ When malignancy is not suspected in a potential differential diagnosis, this type of biopsy may be indicated. This method includes removing the lesion in its entirety. This method lends a more aesthetically pleasing result compared to its other counterparts because no remnants of the lesion are left behind.6
Incisional ─ In cases where malignancy may be included in a differential diagnosis, an incisional biopsy may be warranted. This method involves removing only a small portion of a lesion. In cases of larger lesions or lesions that have several different appearances within the same area, multiple spots of the lesion may be removed to achieve an accurate diagnosis.6
Punch ─ This form of a biopsy can be used to either remove an entire small lesion or a piece of a larger one. In other words, this method can be used as both excisional and incisional, depending on the size of the lesion.6
In this method, a punch biopsy tool is held perpendicular to the lesion, and then it is pushed down and twisted until the tissue is removed.6
Case Study
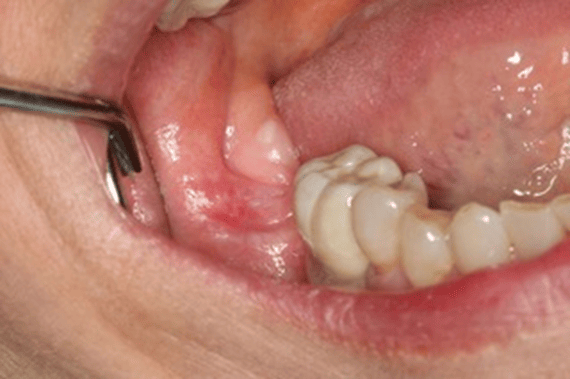
Figure 1 is a photo of a 4×6 mm red and white, flat lesion found on the right posterior mandibular alveolar tissue.
The patient complained of an intermittent “burning” sensation but was otherwise asymptomatic.
Due to the clinical presentation and potential for malignancy, the surgeon chose to perform an incisional biopsy of the area. The pathology report revealed “lichenoid mucositis with epithelial atypia” as the diagnosis.
The patient is not taking either NSAIDs or ACE medications, so this can be ruled out as a cause for the OLL.
As the picture shows, a nearby ceramic crown could be causing the OLL. But this cannot be determined unless the crown is removed and the area is allowed time to heal.
The patient has been informed of the potential for malignancy and is being monitored closely by the surgeon who performed the biopsy. If the surgeon notices any changes to the lesion, a future biopsy may be warranted.
As a side note, the National Institute of Health (NIH) defines atypia as an “abnormality in cells in tissue.”7
Due to the diagnosis containing “epithelial atypia,” the patient is being monitored for changes to the condition and is aware a follow-up biopsy may be needed in the future.
Conclusion
The oral cavity can present with a myriad of conditions and abnormalities that can be nearly impossible to distinguish one from the other. As clinicians, we cannot possibly recognize all of the potential lesions our patients present with but having a good foundation of what’s normal and what isn’t, as well as what can be potentially malignant, can help us give our patients the best level of care.
Because OLLs can be tricky and mimic so many other oral manifestations and lesions, a biopsy still remains the gold standard for diagnosis. If your office doesn’t perform surgical procedures, a referral to another specialist may be warranted.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- McParland, H., Warnakulasuriya, S. Oral Lichenoid Contact Lesions to Mercury and Dental Amalgam—A Review. Journal of Biomedicine and Biotechnology. 2012; 2012: 1-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3409574/
- Kamath, V.V., Setlur, K., Yerlagudda, K. Oral Lichenoid Lesions- A Review and Update. Indian J Dermatol. 2015; 60(1): 102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4318020/
- Vaillant, A.A.J., Vashisht, R., Zito, P.M. (2023, May 29). Immediate Hypersensitivity Reactions. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513315/
- Mills, P.M. Immunological and Inflammatory Aspects of Periodontal Disease Types of Hypersensitivity Reactions. Dentalcare.com.
- Chan, B., Laronde, D.M., Lin, I., et al. Dysplasia Should Not Be Ignored in Lichenoid Mucositis. J. Dent Res. 2018; 97(7): 767–772. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6728589/
- Avon, S-L., Klieb, H.B.E. Oral Soft-tissue Biopsy: An Overview. J Can Dent Assoc. 2012; 78: 1-9. https://jcda.ca/sites/default/files/c75/c75.pdf
- Atypia. (n.d.). NIH: National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/atypia