Yes, you read that title right. But what does that even mean? Generally speaking, people still think the way you get decay is by eating candy and not brushing your teeth enough. They are not completely wrong, but there is more to the story.
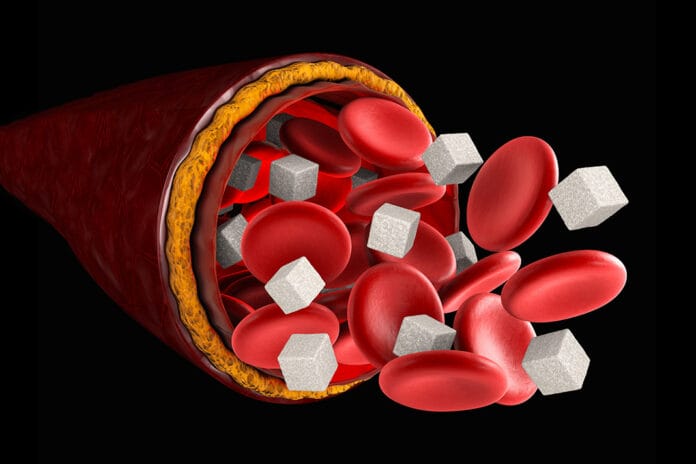
Diabetes: Sugar In Your Blood
According to the International Diabetes Federation (IDF), as of 2021, diabetes affected 537 million, roughly one out of 10 people worldwide. By 2030, it’s estimated 643 million people will be diagnosed with diabetes, and by 2045, the number is expected to rise to 783 million.1 We can probably all agree that is a staggering number, and diabetes is prevalent and only getting more so.
I would bet you can think of at least two or three loved ones living with diabetes right now. Dental hygienists see patients with diabetes nearly every day and are well-versed in the complications patients with diabetes face: 90% of these patients have oral complications such as periodontal disease, xerostomia, decay, candidiasis, altered taste, geographic tongue, fissured tongue, and oral lichen planus.2
Patients with diabetes are more likely to have severe periodontal disease in addition to a higher incidence of disease than those without diabetes. Studies have shown more than 95% of type 2 diabetics suffer from some type of periodontal disease.3 Patients with diabetes are 11 times more likely to have alveolar boneless than those without diabetes.2 The higher the blood sugar, the higher the incidence of, and the more advanced, periodontal disease will be.
Of course, with periodontal disease, the whole body is exposed to inflammation and disease.
Sugar in the Blood Doesn’t Always Stay There
Research has shown with increased blood glucose, there is increased sugar in the crevicular fluid.4 So, it turns out there is still sugar present in the area even if the patient is not snacking on Little Debbie snack cakes all day. When a lot of sugar is hanging around, decay-causing bacteria are constantly being fed. Those bacteria’s waste product is a type of acid that not only demineralizes and breaks down enamel but also sets up an acid-rich environment that both periodontal and caries-causing pathogens love.
In a case like this, we are feeding decay-causing bacteria their favorite food, which in turn gives them their favorite environment in which they thrive. Decay is bound to form. Now, add in a little xerostomia, and we have a full-on recipe for disaster. As hygienists, we have all seen patients that come in with a mouth full of class V decay. It progresses so, so fast, and it is heartbreaking.
From a periodontal standpoint, one of the ways sugar inhibits tissue healing is by impairing immune cells. It alters their ability to move, communicate with, and attack bacteria. The sugar is down-regulating the immune system. When the bacteria can’t be controlled, they multiply exponentially while distributing their endotoxins.
In addition to inhibiting immune cell function, elevated blood sugar inhibits osteoblastic (bone-making) cells and collagen production.5 So, now sugar has not only drastically reduced the ability to fight off an infection, but it has also made it really hard to try to rebuild after the damage has been done. This would explain why patients with diabetes have more alveolar bone loss.
It’s a Two-way Street
Research has shown that diabetes and periodontal disease have a bidirectional relationship, meaning high blood sugar leads to oral infections, and oral infections lead to high blood sugar. The hemoglobin A1C test (HbA1C) is a test that measures an individual’s average blood glucose for the last two to three months. Patients with active periodontal disease have a higher HbA1c level than those with healthy gingiva.6
As far as periodontal disease and blood sugar go, those with periodontal disease have higher long-term blood sugar, a more difficult time controlling their diabetes, are at a higher risk of developing diabetes and gestational diabetes, and have more diabetic complications.7
How does this happen? When periodontal disease is present, the body releases inflammatory cytokines. These cytokines, such as interleukin (IL) and tumor necrosis factor (TNF), increase insulin resistance in addition to continuing to worsen periodontal health. Add bacterial endotoxins to these cytokines, and now pancreatic β cells ‒ cells that produce insulin ‒ are destroyed, which causes even more insulin resistance and blood sugar to rise.2 Patients with diabetes who have periodontal disease have a harder time controlling their blood sugar than patients with diabetes without periodontal disease due to this.
This is yet another great piece of information to share with patients when educating them on the importance of proper home care and frequent recare visits.
Periodontal Treatment: It’s for More Than Gingiva
Research is increasingly linking post-periodontal treatment to lower blood sugar levels.4 Studies have shown those with and without diabetes both improved blood glucose levels after periodontal therapy. Patients with diabetes had better metabolic control after initial treatment and at three- and six-month recare appointments.8
I’m not trying to be a Little Debbie snack cake downer, but we can’t just stay in our ops. We have to reach out and work with other health care providers as a team for the wellness of our patients. Patients with diabetes should not be supported solely by their endocrinologist or primary care provider. Dental practitioners should be part of the team helping patients with diabetes manage their disease.
Before you leave, check out the Today’s RDH self-study CE courses. All courses are peer-reviewed and non-sponsored to focus solely on high-quality education. Click here now.
Listen to the Today’s RDH Dental Hygiene Podcast Below:
References
- Diabetes Around the World. (2021). International Diabetes Federation. https://diabetesatlas.org/
- Ahmad, R., Haque, M. Oral Health Messiers: Diabetes Mellitus Relevance. Diabetes Metabolic Syndrome and Obesity: Targets and Therapy. 2021; 14: 3001-3015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8257029/
- Singh, M., Bains, V.K., Jhingran, R, et al. Prevalence of Periodontal Disease in Type 2 Diabetes Mellitus Patients: A Cross-sectional Study. Contemporary Clinical Dentistry. 2019; 10(2): 349-357. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7145232/
- Indurkar, M.S., Maurya, A.S., Indurkar, S. Oral Manifestations of Diabetes. Clinical Diabetes. 2016; 34(1): 54-57. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714722/
- Gooch, H.L., Hale, J.E., Fujioka, H., et al. Alterations of Cartilage and Collagen Expression during Fracture Healing in Experimental Diabetes. Connective Tissue Research. 2000: 41(2): 81-91. https://pubmed.ncbi.nlm.nih.gov/10992154/
- 6. Sanz, M., Ceriello, A., Buysschaert, M., et al. Scientific Evidence on the Links between Periodontal Diseases and Diabetes: Consensus Report and Guidelines of the Joint Workshop on Periodontal Diseases and Diabetes by the International Diabetes Federation and the European Federation of Periodontology. Journal of Clinical Periodontology. 2018; 45(2): 138-149. https://pubmed.ncbi.nlm.nih.gov/29280174/
- Bendek, M.J., Canedo-Marroquin, G., Realini, O., et al. Periodontitis and Gestational Diabetes Mellitus: A Potential Inflammatory Vicious Cycle. International Journal of Molecular Sciences. 2021; 22(21): 11831. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8584134/
- Faria-Almeida, R., Navarro, A., Bascones, A. Clinical and Metabolic Changes after Conventional Treatment of Type 2 Diabetic Patients with Chronic Periodontitis. Journal of Periodontology. 2006; 77(4): 591-598. https://pubmed.ncbi.nlm.nih.gov/16584339/