Disclosure: We value transparency at Today’s RDH. This quiz is sponsored content from Dentsply Sirona Preventive as part of our sponsored partner program.
Dental handpieces should always be heat sterilized between patients.
According to the Centers for Disease Control and Prevention (CDC) dental handpieces are considered semicritical; “Semicritical items touch mucous membranes or nonintact skin and have a lower risk of transmission; because the majority of semicritical items in dentistry are heat-tolerant, they also should be sterilized by using heat1.”
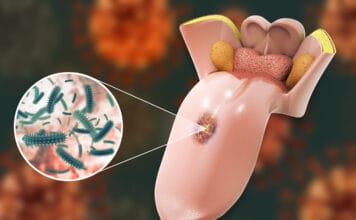
In addition, studies have shown that dental handpieces attached to air and water lines may become contaminated posing a risk for crossinfection2,3. The CDC states “multiple semi-critical dental devices that touch mucous membranes are attached to the air or waterlines of the dental unit1.” The organization recommends clinicians “clean and heat-sterilize handpieces and other intraoral instruments that can be removed from the air and waterlines of dental units between patients1” and “follow the manufacturer’s instructions for cleaning, lubrication, and sterilization1.”
Medical devices sold in the US are cleared by the FDA and that clearance involves reprocessing validation. Manufacturers must document appropriate reprocessing in their Directions for Use (DFU). Always follow the manufacturer’s DFU for cleaning, disinfection and sterilization instructions.
1. Kohn, W.G., Collins, A.S., Cleveland, J.L., Harte, J.A., Eklunt, K.J., Malvitz, D.M. Center for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. MMWR 2003; 52 (Report No. 17). Retrieved from http://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
2. Chin J.R., Miller C.H., Palenik, C.J. (2006). Internal contamination of air-driven low-speed handpieces and attached prophy angles. J Am Dent Assoc. 137(9):1275-80. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16946433
3. Herd S., Chin J., Palenik C.J., Ofner S. (2007) The in vivo contamination of air-driven low-speed handpieces with prophylaxis angles. J Am Dent Assoc. 138(10):1360-5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17908851
An ASTM level 2 (moderate barrier) face mask is appropriate for hand scaling during a dental prophylaxis and rubber cup polishing where moderate amounts of aerosols are produced. An ASTM level 3 face mask (high barrier) is appropriate for high aerosol producing procedures such as the use of an ultrasonic scaling and air polishing.
Both statements are true. The American Society of Testing and Materials (ASTM) specifies performance requirements for medical face masks based on testing for five criteria. These criteria include bacterial filtration efficiency, sub-micron particulate filtration efficiency, fluid resistance to penetration, differential pressure, and flammability.
ASTM Mask Levels1
ASTM 1 (low barrier): For procedures where fluid, spatter, and/or aerosols are produced in low concentration. Examples include taking radiographs, fluoride treatments, patient exams, working in a lab, or disinfecting an operatory.
ASTM 2 (moderate barrier): For procedures where fluid, spatter, and/or aerosols are produced in moderate concentration. Examples include hand scaling during a dental prophylaxis, rubber cup polishing, or sealants.
ASTM 3 (high barrier): For procedures where heavy to moderate levels of fluid, spatter, and/or aerosols are produced. Examples include ultrasonic scaling, use of a Piezo scaler with water, or air polishing.
1. Molinari, J.A., Nelson, P. (July, 2016). Face Masks: What to Wear and When. (Report No. 18) Ann Arbor, Michigan: The Dental Advisor.
Research shows that approximately ___% of metal reusable air/water syringe tips had microbial contamination even after heat sterilization.
The Dental Advisor Biomaterials Research Center investigated heat sterilization outcomes of metal reusable air/water syringe tips. It was found that nearly 10% of metal reusable air/water syringe tips were contaminated with gram-negative rods of water-borne origin after heat sterilization. Further, after heat sterilization of metal reusable air/water syringe tips, particulate material was also visibly observed after sterile trypticase soy broth was aseptically forced through the air/water tip lumens.1
A study published in the Australian Dental Journal by Inger and others, concluded, “Sterilization of non-disposable air/water syringes is not completely effective and rinsing, or the number of uses, does not affect the effectiveness of sterilization. There may be a lower risk of cross-infection from the use of disposable air/water syringe tips, instead of non-disposable ones2.”
1. Molinari, J.A., Nelson, P. (June, 2012). Reusable versus Disposable Air/Water Syringe Tips. (Report No. 13) Ann Arbor, Michigan: The Dental Advisor. Retrieved from https://www.dentaladvisor.com/pdf-download/?pdf_url=images/pdfs/reusable-versus-disposable-air-water-syringe-tips.pdf
2. Inger, M., Bennani, V., Farella, M., Cannon, R.D. (Feb 2014). Efficacy of Air/Water Syringe Tip Sterilization. Australian Dental Journal. 59(1): 87-92. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/adj.12146/pdf
When disinfecting clinical contact surfaces, one wipe with a disinfectant wipe or one spray with a disinfectant is adequate infection control.
Adequate infection control requires clinical contact surfaces to be cleaned first, then disinfected, which requires two wipes, such as in the “wipe, discard, wipe” method. According to the CDC, “Cleaning is the necessary first step of any disinfection process. Cleaning is a form of decontamination that renders the environmental surface safe by removing organic matter, salts, and visible soils, all of which interfere with microbial inactivation. If a surface is not cleaned first, the success of the disinfection process can be compromised. Removal of all visible blood and inorganic and organic matter can be as critical as the germicidal activity of the disinfecting agent.1”
Further, the CDC states, “If barriers are not used, surfaces should be cleaned and disinfected between patients by using an EPA-registered hospital disinfectant with an HIV, HBV claim (i.e., low-level disinfectant) or a tuberculocidal claim (i.e., intermediate-level disinfectant). Intermediate-level disinfectant should be used when the surface is visibly contaminated with blood or other potentially infectious materials1. Cleaning removes large numbers of microorganisms from surfaces and should always precede disinfection2. Not all disinfectant products should be used as cleaners unless the label indicates the product is suitable for such use2.”
In summary, to properly disinfect a clinical contact surface, it must first be cleaned of debris such as blood, saliva, bioburden, exudate, and then disinfected.
1) Kohn, W.G., Collins, A.S., Cleveland, J.L., Harte, J.A., Eklunt, K.J., Malvitz, D.M. Center for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. MMWR 2003; 52 (Report No. 17). Retrieved from http://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
2) Centers for Disease Control and Prevention. (2016, March). Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Retrieved from http://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care.pdf
It is _________ acceptable to heat sterilize, immerse in cold sterile, or high-level disinfect a disposable prophy angle and use it more than once.
It is never acceptable to use a single-use, disposable patient care item more than once. The CDC states, “A single-use device, also called a disposable device, is designed to be used on one patient and then discarded, not reprocessed for use on another patient (e.g., cleaned, disinfected, or sterilized). Single-use devices in dentistry are usually not heat-tolerant and cannot be reliably cleaned. Examples include syringe needles, prophylaxis cups and brushes, and plastic orthodontic brackets. Certain items (e.g., prophylaxis angles, saliva ejectors, high-volume evacuator tips, and air/water syringe tips) are commonly available in a disposable form and should be disposed of appropriately after each use.1 If a semi-critical item is heat-sensitive, dental healthcare personnel should replace it with a heat-tolerant or disposable alternative2.” Always abide by the manufacturer instructions; single use means single use.
1) Kohn, W.G., Collins, A.S., Cleveland, J.L., Harte, J.A., Eklunt, K.J., Malvitz, D.M. Center for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. MMWR 2003; 52 (Report No. 17). Retrieved from http://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
2) Centers for Disease Control and Prevention. (2016, March). Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Retrieved from http://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care.pdf